eligibility check automation
Accurate patient coverage verification – across all EHRs. Fits every EHR – no matter how complicated your processes are.
Integrates with my system? Yes, Epic, Meditech & more.
Setup time? Weeks, not months.
Secure? 100%. HIPAA-compliant, fully encrypted.
No more tedious lookups.
Manual work bloats Cost-To-Collect (CTC)
PHI verification across different systems is tedious and often gets rushed, delayed, or even skipped.
This situation leads straight to re-work, bloated backlog and slower reimbursement.
Agentic AI unlocks capacity and pays for itself
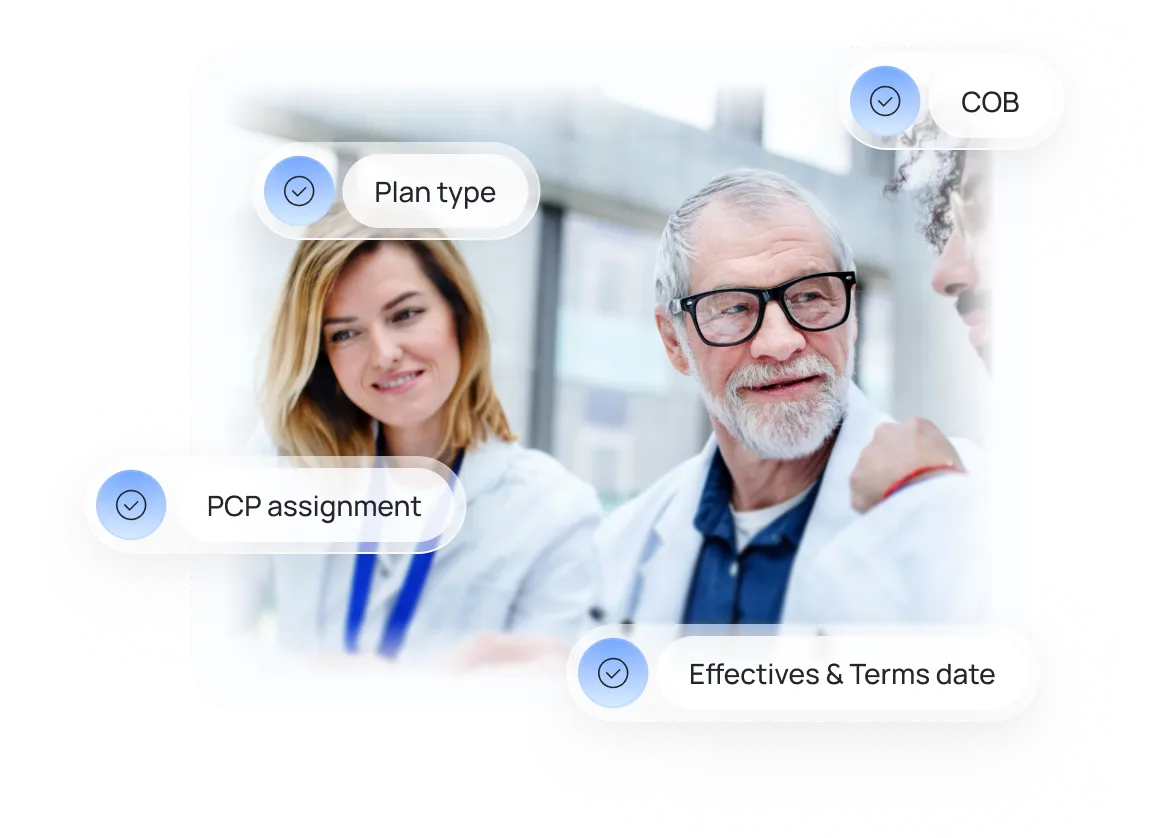
Plan type, effective dates, term dates, PCP assignment, copay / deductible info, COB - our AI agent takes end-to-end care of eligibility checks.
No more manual lookups. No more avoidable costs.
How Eligibility Check Automation Works
Patient Lookup
Eligibility check automation retrieves all required patient insurance information from your EHR to prepare clean identifiers for payer eligibility check. No more PHI hunting.
No more tedious system hopping.

Eligibility Check
Coverage is verified directly with payer systems, confirming active status and patient financial responsibility (copay, coinsurance, deductible) – all without manual work.

Data Logged & Synced
Results like patient coverage and copay/deductibles, are captured, logged, and ready for further processing. Accurate data on every patient, visit and case.


ready to automate your eligibility check process?
Karl – our CTO loves to discuss the ROI. Feel free to book a call with him.
In just 15 minutes, we’ll cut through the noise and see if automation works for you.
Results you can expect.
Proof that speed = cash flow.


Halving Monthly Backlog – Eligibility Automation in Action
This case shows how automated eligibility verification across multiple portals reduces processing time by 90%, cuts manual work by over 90%, and increases verification speed from ~5 minutes to ~1 minute per case.
+50%
Restored capacity. See how AI automation simplified eligibility checks across multiple systems and halved monthly backlog.


100% ROI in just 23 days. We Automated Eligibility Checks!
PTCoA’s case demonstrates how automated eligibility checks can be executed in ~40 seconds, saving 3 FTEs per month and achieving 100% ROI in 23 days with $180K in projected first-year savings.
100%
ROI in just 23 days. Learn about the MVP project which brought +$180,000 worth of savings after year one.

They were easy to get in contact with and the whole collaboration went smoothly. The automation has saved us a considerable amount of time. Everyone in the team confirmed it works fantastically and that it’s freed them up a lot of time.

Thanks to Flobotics, we have increased our sales conversion rate by 3%. The team communicates effectively and is proactive both in the product discovery and development stages. I love the business drive of the team as well as their flexibility and readiness to address all the needs.

Our work with Flobotics helps facilitate the process. It leverages the capabilities of different systems, to make it happen, as no individual system has the capability on its own.We’re very satisfied with their work.
Wait, there is more?
Yes! We also specialize in remaining RCM processes.
Denials Management Automation
Hunts and classifies denials early to stop them from aging out.
Claims Management Automation
Tracks claims and flags denials before they cost you.
Prior Authorization Automation
Automate your PA process. No API required.







.png)