Prior Authorization Automation
Complete PA packets – always aligned with payer rules. Fits every EHR – no matter how complicated your processes are.
Integrates with my system? Yes, Epic, Meditech & more.
Setup time? Weeks, not months.
Secure? 100%. HIPAA-compliant, fully encrypted.
No more documentation gaps.
Manual data intake inflates denials rate (DR)
Missing clinical notes, wrong diagnosis codes, outdated payer criteria - even one gap in the patient’s documentation stalls revenue cycle.
Staffing won’t fix this challenge - consistency will.
Automated PA = complete packet every time.
Our AI Agent gathers required documentation, fills the forms, selects correct CPT/HCPCS codes, understands medical necessity and submits packets through payer portals automatically.
Only true exceptions reach your RCM team.
how prior authorization automation works
Documentation Intake
PA Automation extracts all necessary clinical and coding details from your EHR or intake forms. Each request starts with complete and accurate information – no API needed.
No more tedious system hopping.

Packets Prep & Submission
Our AI agent builds a payer-ready packet every time: correct CPT/HCPCS codes, correct attachments, correct payer criteria, correct format – then submits through the payer portal on its own.
No more guessing what each payer wants.

Real-time Payer Review Tracking
Status changes, additional info requests, pending queues, approval windows - monitors everything and updates your EHR automatically, alerting your team only when human action is needed.
No more delays that turn into denials.

Ready to automate your pre-auth workflow?
Karl – our CTO loves to discuss the ROI. Feel free to book a call with him.
In just 15 minutes, we’ll cut through the noise and see if automation works for you.
Results you can expect.
Proof that speed = cash flow.


90% Faster Packet Submissions | Prior Authorization Automation
This case shows how prior authorization automation eliminated manual data entry for a high-volume genetic diagnostic lab, accelerating patient turnaround and improving competitive advantage without replacing existing systems.
-90%
Faster packet submissions.See how Agentic AI bridged the gap between Laboratory Information Management System (LIMS) and Payer Portals.


85% Faster Submissions, 8+ FTEs Saved | Prior Authorization Automation
This case demonstrates how a fully autonomous AI agent standardized prior authorization submissions across payer portals, eliminating inconsistencies in a large U.S. pain management network.
+8
FTEs saved. Learn how agentic AI freed 8+ FTEs for a leading U.S. health-tech platform and their RCM team.

They were easy to get in contact with and the whole collaboration went smoothly. The automation has saved us a considerable amount of time. Everyone in the team confirmed it works fantastically and that it’s freed them up a lot of time.

Thanks to Flobotics, we have increased our sales conversion rate by 3%. The team communicates effectively and is proactive both in the product discovery and development stages. I love the business drive of the team as well as their flexibility and readiness to address all the needs.

Our work with Flobotics helps facilitate the process. It leverages the capabilities of different systems, to make it happen, as no individual system has the capability on its own.We’re very satisfied with their work.
Wait, there is more?
Yes! We also specialize in remaining RCM processes.
Denials Management Automation
Hunts and classifies denials early to stop them from aging out.
Claims Management Automation
Tracks claims and flags denials before they cost you.
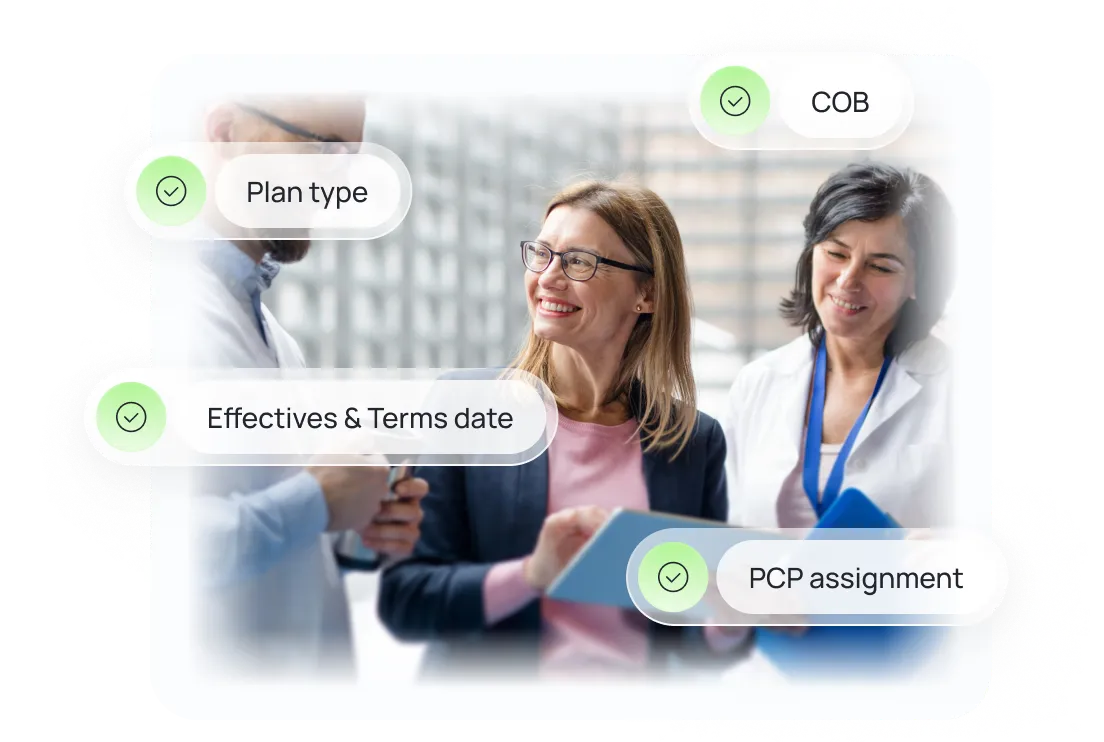
Eligibility Check Automation
24/7 patient coverage verification - all without human supervision






