the way we price shouldn’t be a secret
Your process may be complex, but understanding the cost shouldn’t be.
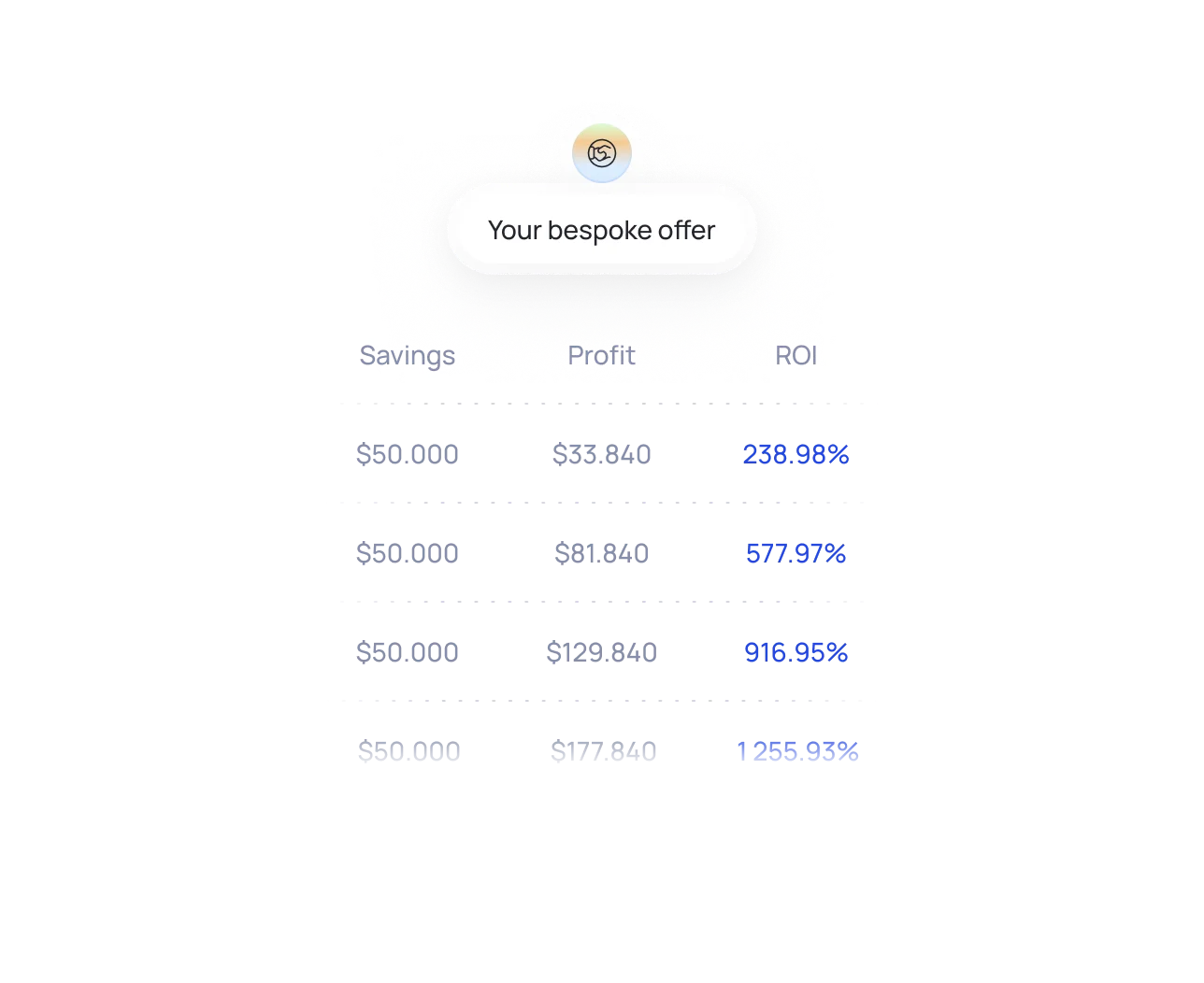
what you can expect to pay
Typical RCM automation projects fall between: $20,000 – $35,000.
Below are real examples from healthcare clients who used the same automation approach you will.
Eligibility automation project
Unattended patient eligibility validation - prior to service
Denials resubmission for the laboratory.
Denials resubmission for the laboratory EHR-to-claim data pipeline automation
Pre-auth automation project for cancer treatment clinic.
PA packets automatic completion aligned with payer rules.





how the process works
We don’t use call screeners. You speak directly to someone who builds automations.
A real walkthrough - not a questionnaire. (30 - 60 minutes based on complexity of the process)
Tech stack, complexity, volume, potential ROI, edge cases.
We answer any questions and show you precise estimates. No surprises. No upsells. No vague ranges.
what affects pricing?
Workflow complexity
Number of systems involved
Volume or frequency
Reporting or audit needs
Data availability
Special payer/clinic rules
get pricing for your project
We can give you a rough ballpark in the first 15 minutes of call one.
We’ll cut through the noise and see if automation works for you.