Denials Management Automation
Resubmissions done right – approvals without manual rework. Fits every EHR – no matter how complicated your processes are.
Integrates with my system? Yes, Epic, Meditech & more.
Setup time? Weeks, not months.
Secure? 100%. HIPAA-compliant, fully encrypted.
No more tedious rework.
Denial Rate (DR) is always too high.
In many cases, overburdened RCM teams discover the issue too late to recover the payment.
Missing documentation, coding mismatches, expired PAs – even one incorrect detail costs rework, causes delayed reimbursement or ends up denied.
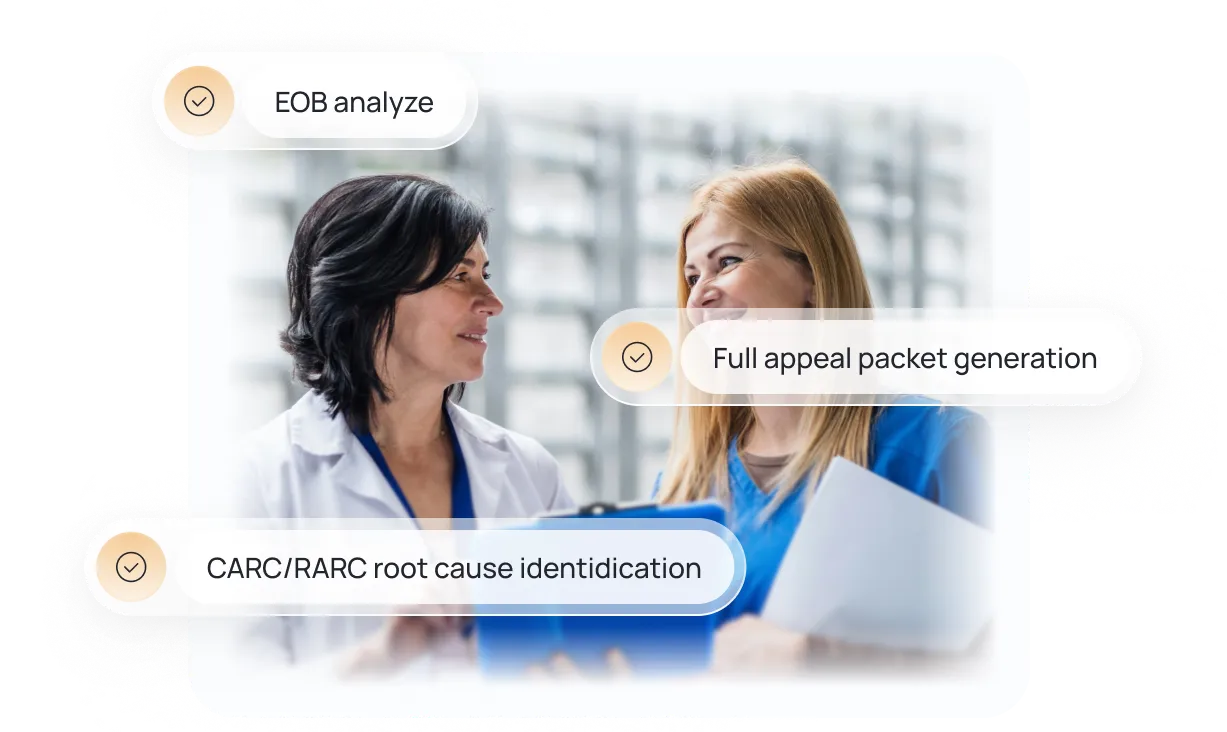
Agentic AI is the fastest path to reimbursement
Our AI Agent analyzes each EOB, identifies the CARC/RARC root cause of denial, and generates full appeal packets for automatic denial resubmission.
No more crunch time. No more tedious rework.
How Denials Management Automation Works
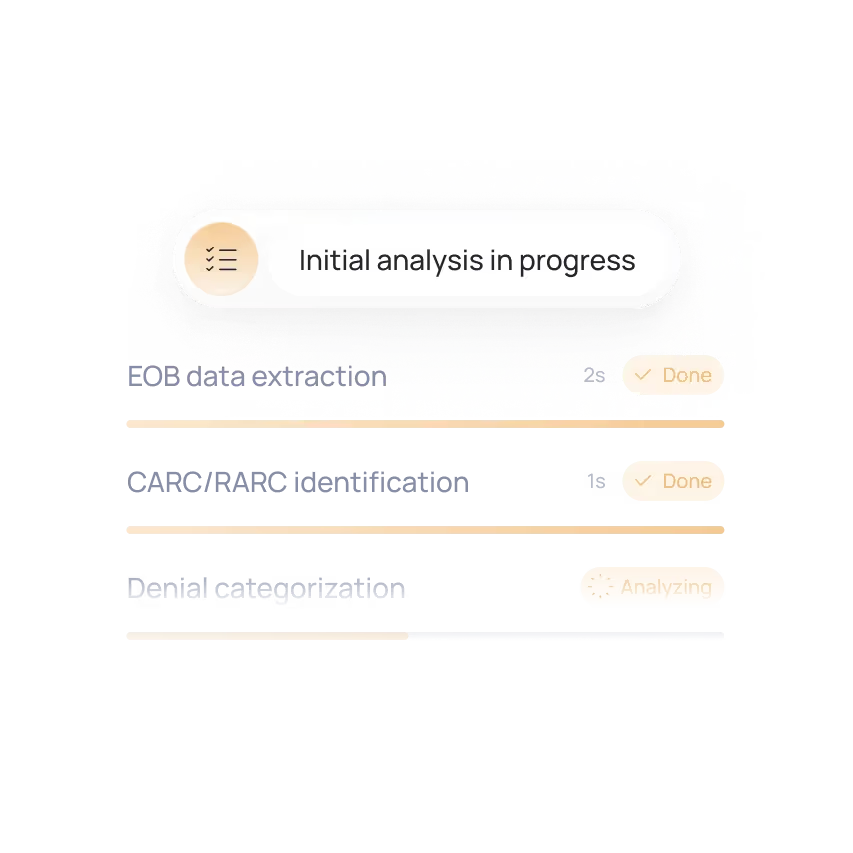
Decoding Denial Cause
Explanation of Benefits (EOB), the CARC/RARC reasons identification and denial categorization – all take only a few seconds.
No more digging through codes, portals, and payer PDFs.

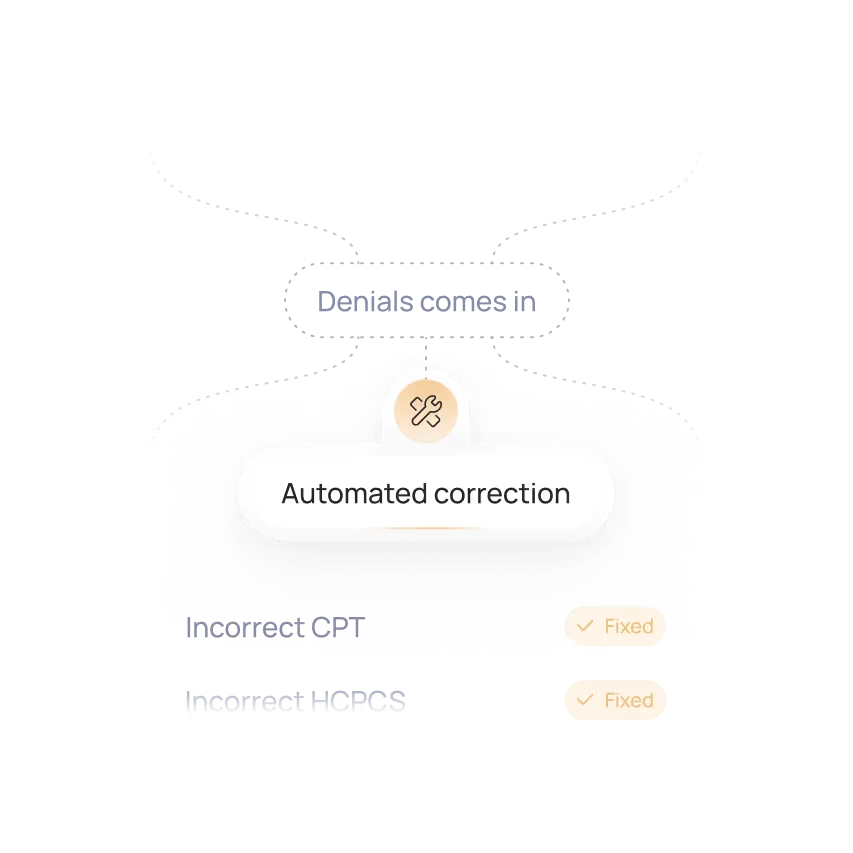
Root Cause Correction
Denials are often linked to missing documentation, incorrect CPT/HCPCS/ICD-10 combinations, or payer-specific requirements – all predictable, rule-based issues can be corrected automatically.
No more missing notes. No outdated info.

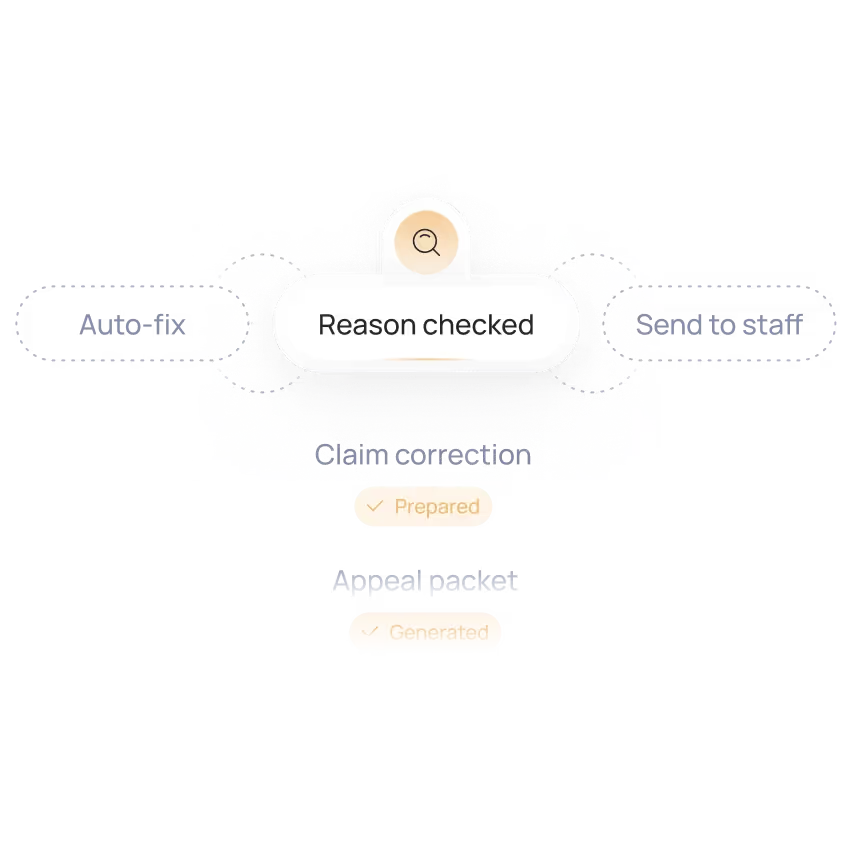
Auto-resubmission and Tracking
Matches the denial to missing documentation, coding discrepancies, or payer-specific requirements – and prepares the corrected claim or appeal packet automatically.
Lower workload, faster resolution, more consistent reimbursement.

Ready to automate your denials management workflow?
Karl – our CTO loves to discuss the ROI. Feel free to book a call with him.
In just 15 minutes, we’ll cut through the noise and see if automation works for you.
Results you can expect.
Proof that speed = cash flow.


+$50K Saved in 1 Month | AI Agent For Denials Management
This case demonstrates how AI-driven denial automation eliminated ~90% of manual rework, reduced claim processing time from ~6 minutes to ~30 seconds, cleared 80% of a 3,000-record backlog in three weeks, and delivered $90K+ in savings with 500+ hours saved monthly.
+$50K
Saved in 1 Month. Discover AI automations that reduce 90% of manual re-work for RCM teams.


Up to 80% Higher Throughput in RCM – Denials Management Automation
PathGroup’s case shows how automated denial handling across athenahealth and PathSys reduced processing time from ~10 minutes to ~55 seconds, cleared backlogs to near-zero, and scaled to ~300 automated resubmissions per day.
98%
Reduction in manual claim prep. See how an automated EHR-to-claim data pipeline removed up to 250 hours per week of manual RCM work.

They were easy to get in contact with and the whole collaboration went smoothly. The automation has saved us a considerable amount of time. Everyone in the team confirmed it works fantastically and that it’s freed them up a lot of time.

Thanks to Flobotics, we have increased our sales conversion rate by 3%. The team communicates effectively and is proactive both in the product discovery and development stages. I love the business drive of the team as well as their flexibility and readiness to address all the needs.

Our work with Flobotics helps facilitate the process. It leverages the capabilities of different systems, to make it happen, as no individual system has the capability on its own.We’re very satisfied with their work.
Wait, there is more?
Yes! We also specialize in remaining RCM processes.
Claims Management Automation
Tracks claims and flags denials before they cost you.
Prior Authorization Automation
Automate your PA process. No API required.
Eligibility Check Automation
24/7 patient coverage verification - all without human supervision






