+$50K Saved in 1 Month | AI Agent For Denials Management
Discover AI automations that reduce 90% of manual re-work for RCM teams.

Project Scope
At the beginning of 2025, a recognizable medtech startup from California contacted us for two things:
- Automation opportunities audit
- Denials management automation
They mainly focus on disease detection improvements and molecular diagnostics, but as it is common in modern times, their growth path leads through technological improvement - in this case process automations.
Main Challenge | Scaling
Scaling Revenue Cycle Management (RCM) operations is quite challenging.
Growing denial rates, delayed reimbursements, overextended staff - we bet that sounds familiar. It’s a very common case among medtech startups in the U.S.
After all:
Higher claims volume = Back-office pressure
In this case, the main part of the workload consisted of manual correspondence, data re-entry, and reconciliation across Xifin and payer portals.
On top of that, each day, more than tens of new claim denials popped up. They all required handling - entirely by hand. When UnitedHealthcare introduced PIB12 and PI96 denial codes, the claims backlog surged past 3,000 records.
Each one required validation, reconciliation, and resubmission.
What would your company do in such a situation?
Hiring more people wouldn’t change much. After all, the main goal was to scale the operations, not to double the digits on the charts, right?
Their team quickly realized that.
The Bottom Line
The MedTech startup we're describing needed a scalable way to process data and accelerate reimbursements.
Not only to keep the momentum, but most importantly, to secure & stabilize the revenue stream - all without bloating the CTC metrics.
They instantly knew that their situation requires:
- Improved operational capacity,
- Cost To Collect (CTC) optimization,
- Precise end-to-end denial handling.
In short:
The investment in automation was inevitable.
Solutions | AI Automation to the Rescue!
To scale efficiently, they needed automation that could handle both:
- structured processes (like Xifin workflows and payer integrations)
- unstructured processes (such as documents processing, correspondence, etc.).
The main goal of our task was clear – eliminate the repetitive, time-consuming tasks that were bogging down the RCM team.
So far, the cooperation resulted in the following targeted AI automations:
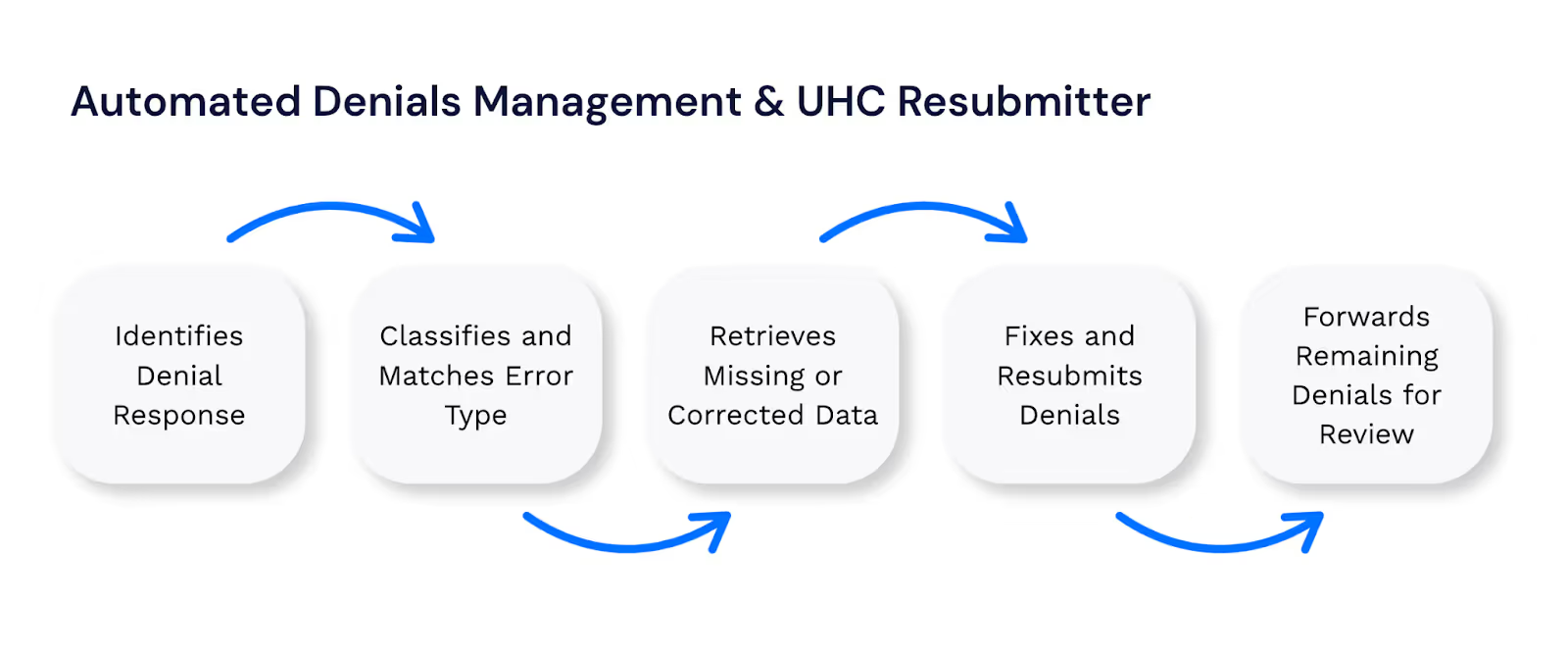
Denials Handling System
At first, we’ve decided to build an automation system that takes over the repetitive and error-prone parts of claim handling.
We aimed to find and classify denial types, pull missing or corrected data, fix claims, and resubmit them to payer portals automatically.
Only the complex cases that need human input were meant for the RCM team.
We designed the entire flow to move claims forward without manual work.
How Denials Handling Automation works:
Results:
Denials that used to delay payments for days are now resolved in seconds - giving the team more time to focus on the cases that really need their attention.
- Manual rework eliminated for 90% of cases
- Only the last 10% routed to staff
- Small human errors completely removed
PIB12/PI96 Denial Reconsiderations
Remember the piling up PIB12/PI96 denials issue?
A backlog of over 3,000 claims created an urgent need for another automation - so we moved fast.
Within three weeks, the PIB12/PI96 Denial Reconsiderations automation cleared 80% of the backlog and then became a daily automation.
Here’s how it works:
The automation retrieves denied accessions from Xifin, extracts key details, and downloads the related medical records. It then matches each record to the correct UnitedHealthcare (UHC) claim, uploads the required documentation, and submits the reconsideration request.
Once complete, the system updates the claim status in Xifin and sends execution summaries via Slack and email - keeping the RCM team fully informed.
Today, the automation handles around 50 denials per day, covering reason codes M127, N705, PI252, CO252, N393, and OA252.
The success of this initiative also led to ongoing collaboration with UHC.
Results:
- Manual denials handling reduced from 6 min → 30 sec per case
- ~4 hours saved daily
- More RCM FTEs for complex appeals
Resubmiton Module Automation
During PIB12/PI96 testing, multiple claims required re-submission.
The scope was extended to include a resubmission module, developed in just 1 week, combining API efficiency with GUI flexibility.
It was also re-usable for future denial types - making it future-proof.
Results:
- ~1,200 failed claims automatically updated
- ~120 hours saved for the RCM team
- Additional 2 hrs/day saved on PIB12/PI96 reconsiderations
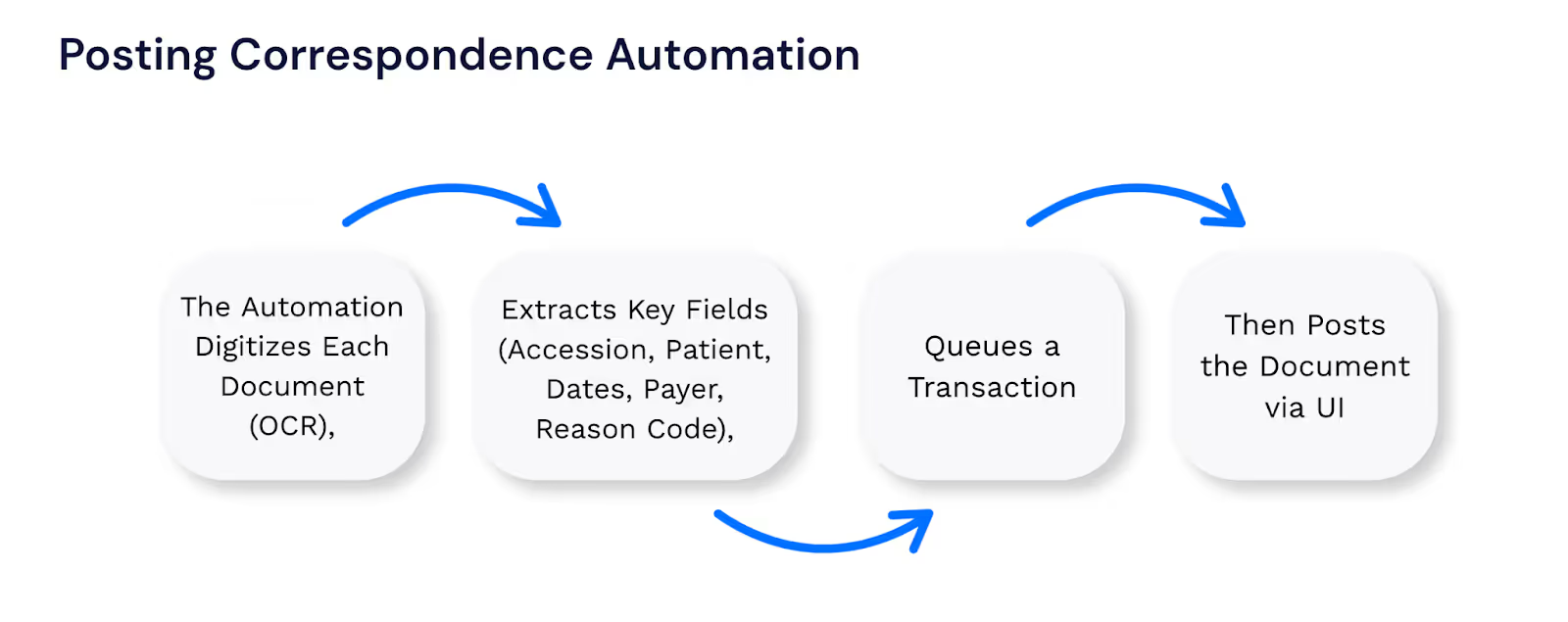
Posting Correspondence Automation
The described startup expanded their automation to mainly handle payer correspondence using UiPath and AI.
The goal for our automation was clear:
Process all of incoming mail the same day - with no human input.
Hand in hand with their internal IT team we’ve created a system that digitizes physical mail, sorts documents into Google Drive, and reads and extracts key data automatically.
It was also designed to map reason codes and update claim records in Xifin, keeping everything accurate and up to date without manual effort.
How Posting Correspondence Works?
Results:
- 95% less manual post correspondence processing
- Accelerated claim adjudication and payment
- 24/7 AI mailroom - no extra headcount
- Billing team redirected from admin work to core finance activities
The Outcomes
So far, denial management and post correspondence automation has delivered promissing results.
Our partner saved above $90,000 to date, while replacing over 2,300 hours of manual work with fully automated processes.
Nearly 90% of all manual rework has been eliminated, leaving only the most complex 10% of cases for staff review.
Within just three weeks, automation cleared 80% of a 3,000-claim denial backlog, improving operational throughput.
Processing time for each claim has dropped by 90%, from six minutes to roughly 20–30 seconds, and reimbursement cycles have been shortened by four days.
The transformation has also changed how the team works.
Freed from repetitive tasks, team members now focus on higher-value analysis, appeals, and strategic improvements.
Summary
This particular case shows that investing in AI automation and RPA brings multiple profits.
With 15 automations operating so far (more underway), the improvement is visible almost across every part of the revenue cycle management field.
Current roadmap includes Availity integration, LLM-based automation for HR, and expanding AI to contract management.
Which brings us to the following point:
At Flobotics we focus exclusively on automating what matters most in U.S. healthcare revenue cycle management - no generic bots here.
Ready to scale without growing headcount? Let’s talk!
Let’s talk. In just 15 minutes, we’ll cut through the noise and see if automation works for you.