$16 million—that’s the highest HIPAA non-compliance penalty to date, paid by Anthem Inc., one of the largest health benefits companies in the US. In 2015, cyber-attackers exploited Anthem’s insufficient access control procedures, stealing the ePHI of nearly 79 million policyholders.
In a more recent healthcare data violation, a 2022 ransomware attack targeted at a printing and mailing vendor, OneTouchPoint, affected 34 healthcare organizations that were the company’s customers. As a result, records of over 2.5 million people were compromised.
These and dozens of other cases each year share the same root cause: non-compliance with safety measures required by acts such as HIPAA or the HITECH Act. Exorbitant penalties aside, failing to adhere to the increasingly complicated healthcare regulations entails risks much more severe than financial losses.
Luckily, with the help of RPA-based compliance automation, meeting legal requirements is more effortless than ever. Why? And what regulations are these? You’ll find it out in a moment—welcome to our overview of the most critical healthcare-related regulations in the US and how RPA can help you meet them.
Why is healthcare compliance important?
Despite the million-dollar fines and all the talk about the importance of compliance, healthcare data breaches had been on a 14-year rise until a slight decrease in 2022. So, before discussing regulations, let’s see what makes following them vital.
Security breaches
While the large cases involving millions of policyholders get the most media coverage, they are far from the only ones. The US Department of Health and Human Services’ Office for Civil Rights (OCR) reports hundreds of healthcare regulation breaches yearly, with an all-time high of 715 in 2021 alone.
Costly fines
Settlements and monetary penalties cost healthcare organizations millions of dollars each year. Just in 2023, non-compliance fines amounted to more than $3 million, which is still relatively small compared to most previous years.
Lower patient care quality
Financial losses resulting from non-compliance can severely disrupt the operational capabilities of your healthcare organization. Lower funds mean reduced investments, fewer equipment upgrades, discontinued services, and even layoffs.
Patient distrust
Though eroding trust can’t be measured with numbers, it’s the ultimate consequence of non-compliance. The blow to reputation following a sensitive data breach is hard to recover from, leading to further financial losses.
Legal Requirements in the US Regarding Compliance
As healthcare and data technologies developed, many policies were implemented to ensure healthcare services’ efficiency and protect sensitive information. Today, multiple laws regulate healthcare data sharing and safeguarding in the US. Here are some of the most essential ones.
Health Insurance Portability and Accountability Act (HIPAA)
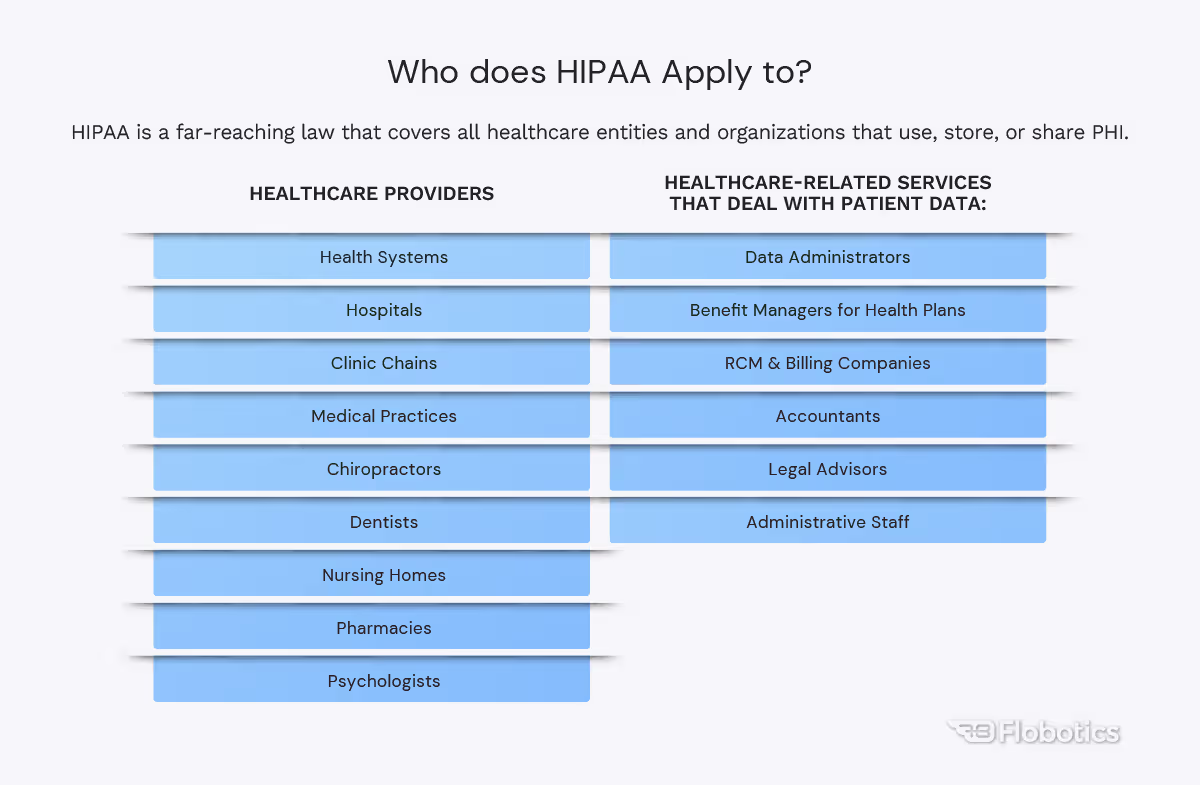
The most well-known healthcare data regulation, HIPAA, was established in 1996 to govern the use and sharing of patient records in all formats, whether verbal, written, or electronic. Under HIPAA, the Department of Health and Human Services (HHS) sets boundaries on using and sharing health information, safeguards to protect patients’ records, and penalties for violations.
Eventually, additional rules were established to build on HIPAA. The HIPAA Privacy Rule introduced nationwide standards for securing, using, and sharing PHI, and it outlines how entities can use these records without a patient’s explicit authorization. It also gives patients control over their information, including the right to examine, obtain, and issue copies of their health records and to request necessary corrections.
HIPAA Security Rule puts these standards into action, requiring providers to assess risk and then implement appropriate administrative, physical, and technical measures to keep electronic PHI (ePHI) safe.
Health Information Technology for Economic and Clinical Health Act (HITECH)
As EHR breach attempts grew more sophisticated, new regulations were needed to help entities fight them, which led to the creation of the HITECH Act in 2009.
HITECH Act focuses on standardizing EHRs, their security, and sharing. Under HITECH, ePHI can only be transferred using secured channels, not traditional methods like emails. The regulation requires providers to notify patients about unauthorized access or use of their records.
HITECH also obliges HHS to conduct regular audits and exact penalties on non-compliant providers. Another goal of the HITECH Act is to promote the adoption and use of EHR—to encourage providers to switch to electronic data systems, the law offers financial incentives.
Affordable Care Act (ACA)
The overarching goal of ACA, introduced in 2010, is to make healthcare insurance accessible and affordable to more people. This is done by subsidizing health services for lower-income households, expanding the coverage of the Medicaid program, and requiring subject businesses to offer minimum essential health insurance to their employees.
Patient Safety and Quality Improvement Act (PSQIA)
Released in 2005, PSQIA is a reporting system designed to reduce costly and dangerous medical errors. PSQIA created a framework for establishing patient safety organizations (PSOs) that could collect and analyze patient information from healthcare providers. Importantly, PSQIA warrants the confidentiality of patient records featured in the reports, allowing for anonymized and safe sharing of sensitive data.
Emergency Medical Treatment and Active Labor Act (EMTALA)
As another law concerned with increasing the availability of healthcare, EMTALA requires hospitals to run preliminary screenings of admitted uninsured or Medicaid-covered patients in emergency cases before transferring them to public hospitals.
Under EMTALA, patients can only be transferred if these screenings determine that their condition is stable or if the medical benefits of moving the patients outweigh the risks. From the data point of view, hospitals must also provide copies of patient’s medical records to the facility they are transferred to.
What tasks can you streamline with compliance automation?
Meeting all legal requirements involves processing huge volumes of data between test results, patient personal data, insurance claims, and other documents. Due to that, compliance-related workflows can take a heavy toll on your time and resources.
However, the same reliance on data processing makes many tasks the perfect candidates for automation using technologies like RPA. So, what can you relegate to healthcare compliance automation?
- Moving medical records — whether you need to update your EHR, migrate data to a cloud-based one, unify disjointed datasets into a centralized source, or simply retrieve specific patient records, RPA can automate mundane healthcare tasks involving moving medical data.
- Data entry — RPA is equally apt at filling standardized paperwork and preparing the necessary documents continuously and with a near-zero error rate.
- Document digitization — with the help of optical character recognition (OCR), RPA can read even paper-based documents, allowing organizations to convert medical documentation into digital format quickly.
- Monitoring and auditing — RPA allows providers to monitor incoming records and run routine compliance checks of massive datasets without stretching their back-office staff too thin.
- Reporting — once the check is complete, RPA will compile its findings into a report to share with the selected team members.
- Automated alerts — should RPA bots detect errors or inconsistencies that could lead to non-compliance, they will automatically flag them and notify your staff.
- Access monitoring — bots can be programmed to monitor PHI access and identify deviations from the usual pattern, indicating potential breaches, theft attempts, and other dangers.
- Suggesting improvements — automation solutions can inspect current processes at higher levels of advancement to find inefficiencies and identify potential improvements.
What are the benefits of using compliance automation?
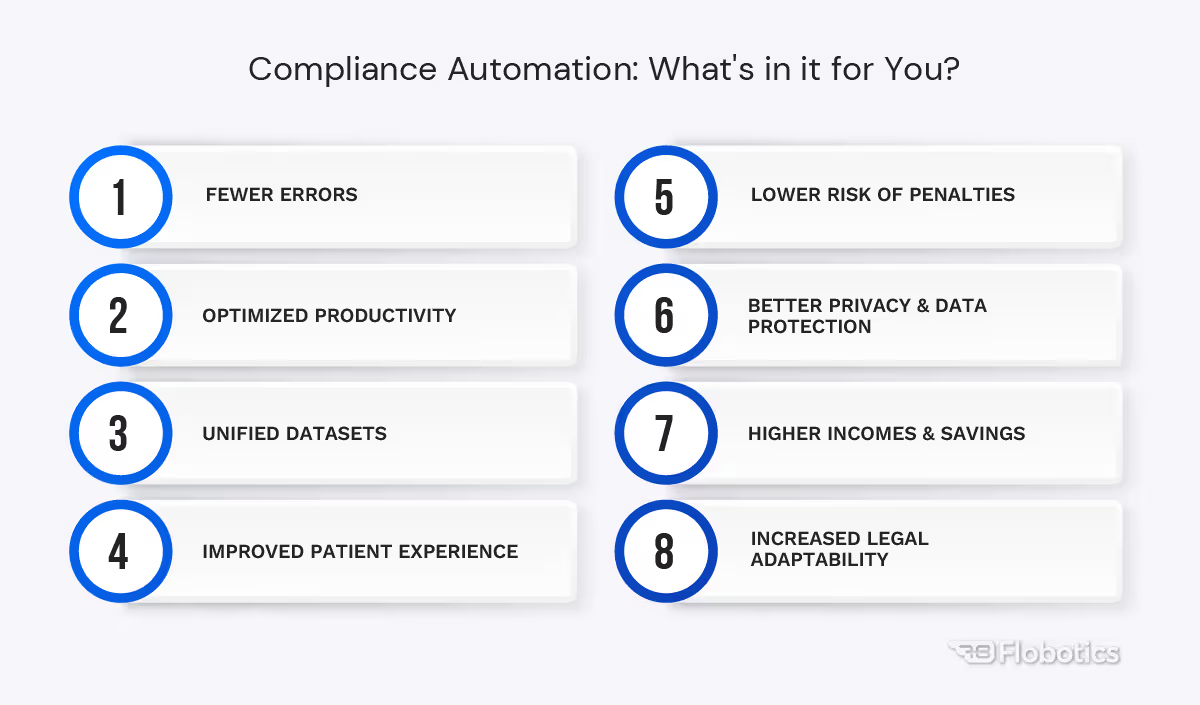
Automating compliance-related tasks makes it much easier for healthcare organizations to meet all legal requirements, but the benefits of RPA in healthcare don’t end there.
Improved accuracy
By automatically handling error-prone manual tasks like copy-pasting medical data, filling in documentation, or moving files containing sensitive records, RPA helps bring the rate of human error down almost to zero.
Reduced risk of penalties
RPA limits the risk of a data breach in several ways, thus reducing the likelihood of receiving violation fines. And, in the unlikely case that security is compromised, showing diligence helps settle for a lower penalty.
Centralized data
Automated data operations make it much easier for companies to unify all their records and avoid siloed datasets. This, in turn, allows for better safety measures, monitoring, access control, and, ultimately, higher compliance.
Enhanced data security and privacy
RPA bots can monitor sensitive datasets around the clock and, unlike humans, won’t overlook suspicious activity due to distraction. They can also be used to implement internal self-assessment systems and prevent external controls from government agencies.
Increased efficiency
Regulatory tasks require a lot of effort, diverting your employees from higher-impact duties. With RPA, they can devote more of their time and energy to innovation or strategic decisions.

Financial gains
Automation lowers your spending by cutting operational costs and helping you avoid fines. Additionally, it can boost your earnings by increasing productivity and allowing you to accept more patients.
Quicker adapting to shifting regulations
Adjusting your compliance procedures to regulatory changes requires retraining staff and changing processes, causing confusion, costing time, and leading to potential errors. At the same time, everything that RPA bots need to run the updated procedures is one-time reprogramming and testing.
Better patient experience and trust
Ultimately, it’s not just your organization that benefits from all these improvements. Compliance automation translates into faster and more reliable care delivery for your patients and certainty that their sensitive information is kept safe.
Compliance automation examples
Global industry leaders are already using RPA for healthcare automation. This includes some of our clients.
Faster and smarter medical billing with RPA
Transferring medical records between all entities involved in the patient journey safely and efficiently is a long-term healthcare challenge.
For that, we created dedicated SuperPay accounts for each of their clients and then designed RPA bots that automatically logged into that account and scanned each provider’s EHR database for eligible patients. The bots would also send automated SuperPay invites to these patients and handle a range of other activities, such as patient account creation, payment method updates, or retrieving claim details. The benefits were threefold: less time spent on each patient billed, faster data transfers, and reduced cost.
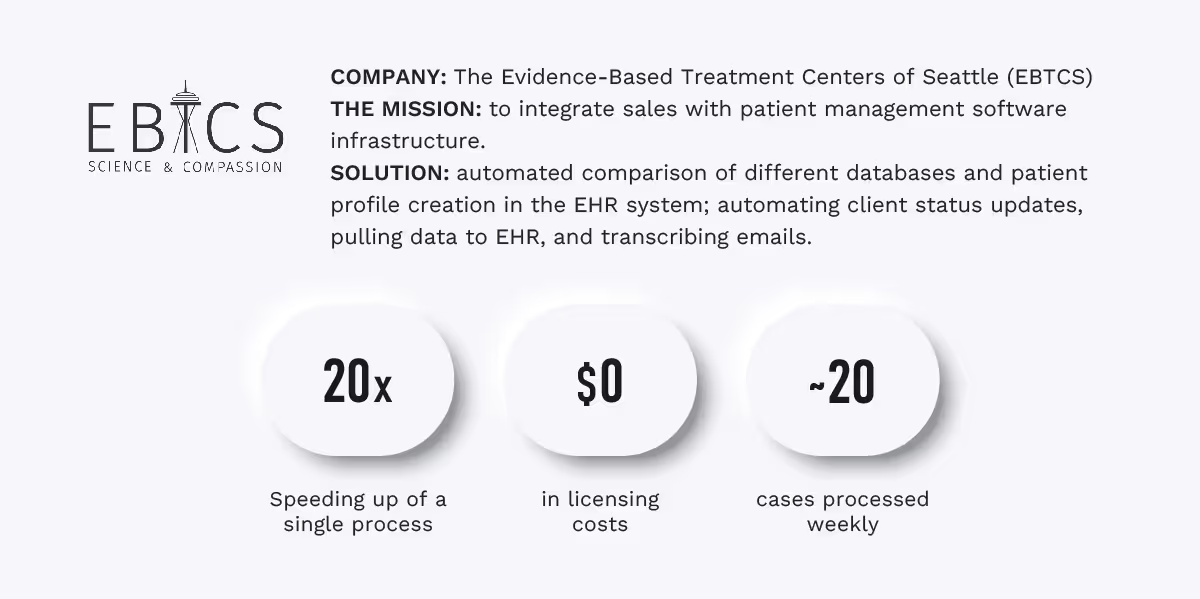
Bringing multiple EHRs together
Integrating healthcare systems with third-party software proved challenging for the Evidence-Based Treatment Centers of Seattle (EBTCS), a network of mental health centers. In this case, their EHR, Valant, lacked publicly-accessed API, preventing EBTCS from connecting it to Salesforce, and effectively forcing its staff to move records manually.
Following a close analysis of the system, we suggested a Python automation solution, Robocorp. Using the tool, we created a bot that regularly compared Valant and Salesforce databases and automatically created patient profiles in the EHR system based on sales data. It doesn’t end there: the bot also updates Salesforce client status, pulls data from Valant and documents from Salesforce to EHR, transcribes emails, and notifies team members of relevant changes. All that allows for seamless communication between EHR, the sales platform, and EBTCS staff.
Healthcare RPA: your way to compliance
As healthcare is becoming more reliant on data and technology, regulations must keep up to warrant the safety and quality of healthcare services. The same applies to providers, who, through compliance, can directly improve their effectiveness and integrity.
Compliance automation and RPA offer healthcare organizations a shortcut to achieving this goal with the added benefits of increased productivity, savings, and optimized operations. Curious to find out more? Drop us a line.
Like the article? Spread the word
Streamlining Compliance: Automation Strategies in Healthcare
In the high-stakes world of healthcare, compliance is not just a legal obligation—it is a cornerstone of patient trust and safety. However, as regulations like HIPAA and GDPR evolve, manual oversight is becoming a liability. Compliance automation transforms this burden into a strategic advantage, replacing spreadsheets and manual audits with real-time monitoring and AI-driven insights.
Understanding Healthcare Compliance Requirements
The healthcare regulatory environment is a complex web of federal, state, and international laws. Effective automation begins with identifying which of these frameworks apply to your specific operations.
Key Regulations and Standards
- HIPAA (Health Insurance Portability and Accountability Act): The primary U.S. law protecting patient health information (PHI). It mandates administrative, physical, and technical safeguards.
- HITECH Act: An extension of HIPAA that promotes the "meaningful use" of health IT and introduces stricter penalties for data breaches.
- GDPR (General Data Protection Regulation): Essential for any provider handling the data of EU citizens. Unlike HIPAA, GDPR includes the "right to be forgotten."
- 21st Century Cures Act: Focuses on interoperability and preventing "information blocking," ensuring patients have easy access to their electronic health information (EHI).
Compliance Documentation Necessities
To survive a regulatory audit, "doing the work" isn't enough; you must prove it. Mandatory documentation includes:
- Risk Assessments: Regular evaluations of vulnerabilities in PHI security.
- Business Associate Agreements (BAAs): Contracts ensuring third-party vendors adhere to the same security standards.
- Policy Attestations: Proof that every employee has read and understood compliance protocols.
The Landscape of Compliance Automation Technologies
Modern automation tools do more than store files—they act as a "digital nervous system" for your organization’s data.
Types of Automation Tools Available
- GRC Platforms (Governance, Risk, and Compliance): Centralized hubs like Vanta or Drata that map controls across multiple frameworks simultaneously.
- Specialized Healthcare GRC: Tools like ComplyAssistant or MedTrainer built specifically for clinical environments with pre-loaded HIPAA templates.
- Point Solutions: Dedicated tools for specific tasks, such as Paubox for encrypted email or Jotform for HIPAA-compliant patient intake.
Features to Look For in Automation Solutions
- Continuous Control Monitoring (CCM): Instead of an annual check-up, CCM provides 24/7 alerts if a security configuration (like an open AWS bucket) drifts out of compliance.
- AI-Powered Evidence Collection: Automatically pulls logs from your EHR, cloud providers, and HR systems to populate audit folders.
- Multi-Framework Mapping: The ability to perform one action (e.g., setting a password policy) and have it automatically satisfy requirements for HIPAA, SOC 2, and ISO 27001.
Implementing Compliance Automation: A Practical Guide
Moving from manual to automated systems requires a structured roadmap to avoid operational friction.
Assessing Your Organization's Readiness
Before buying software, evaluate your current maturity. Do you have documented policies? Are your data sources (EHR, Billing, HR) accessible via API? Small practices may only need point solutions, while large health systems require a full GRC suite.
Step-by-Step Implementation Framework
- Inventory Data Assets: Identify where PHI lives and how it flows through your system.
- Select a Lead Framework: Start with your highest priority (usually HIPAA) before layering on others.
- Integrate Systems: Connect your automation tool to your tech stack (Microsoft 365, EHR, Cloud Hosting).
- Automate Workflows: Set up triggers for recurring tasks like quarterly access reviews and annual training.
- Audit and Refine: Use the tool’s dashboard to identify gaps and remediate them before an official audit.
Measuring Success and ROI of Automation
Measuring ROI in compliance is about cost avoidance and operational speed.
- Direct Savings: Reduced hours spent on manual evidence collection (often 40–60% less time).
- Risk Mitigation: Avoiding HIPAA fines, which can reach over $2 million annually for severe violations.
- Operational Velocity: Faster onboarding of new clinical staff and quicker vendor security reviews.
Challenges and Solutions in Compliance Automation
Overcoming Resistance to Change
The biggest hurdle is often human, not technical. Staff may view new monitoring tools as "micromanagement."
- Solution: Frame automation as a tool that protects the staff's license and reputation. Highlight how it removes the "paperwork" they dislike, allowing them to focus on patient care.
Addressing Common Implementation Pitfalls
- The "Set It and Forget It" Trap: Automation is not a replacement for a Compliance Officer.
- Fix: Schedule monthly "dashboard reviews" to address alerts that the system cannot fix on its own.
- Data Silos: If your billing software doesn't talk to your GRC tool, you have a blind spot.
- Fix: Prioritize tools with native integrations or robust APIs for your specific EHR.
Future Trends in Compliance Automation in Healthcare
Innovations on the Horizon
- AI Compliance Coaches: Conversational AI that can answer staff questions about specific policies in real-time, reducing the burden on HR.
- Predictive Risk Scoring: Using machine learning to predict which department is most likely to suffer a breach based on behavioral patterns.
Preparing for Regulatory Changes
Regulatory bodies are moving toward Real-Time Reporting. In the future, "audits" may not be scheduled events but continuous data streams shared directly with regulators. Investing in automation today ensures your infrastructure is ready for the "live" compliance era of 2026 and beyond.
Would you like me to create a comparison table of the top 5 compliance automation tools specifically for small-to-medium healthcare providers?











.jpg)


