Up to 80% Higher Throughput in RCM – Denials Management Automation
See how we automated PathGroup’s systems and connected it with a custom laboratory information system data exchange.

About PathGroup
PathGroup is one of the largest physician–led pathology and laboratory service providers in the U.S.
They serve more than 95 hospitals and thousands of physician groups nationwide and process thousands of claims a day.
In the past, their RCM team was manually operating on two hard to integrate systems:
- athenahealth (previously IDX) – a major legacy billing and patient management platform for patient charges handling, claim generation, and payer reporting.
- PathSys Laboratory Information System – private proprietary legacy EHR software, built in – house to manage diagnostic data, lab results, and test coding at scale.
The lack of integration between the two systems created a growing denials backlog, which soon became a serious operational bottleneck.
Main Challenge | Denials Management
Before automation, processing a denied claim typically required 10–15 minutes of manual work.
Manual cross–checks, data correction, claim resubmission… At scale, this volume made it impossible for the team to keep up.
At the top of that, constant rework generating costs, delayed time to reimbursements, and prolonged Account Receivables (AR).
Hiring more staff would only inflate Cost–To–Collect (CTC) instead of solving throughput.
In short:
Automation was inevitable.
Solutions | AI Automation to the Rescue!
After breaking down their revenue cycle piece by piece, we knew that PathGroups situation required:
- Improved operational capacity,
- Cost To Collect (CTC) optimization,
- Precise end– to– end denial handling.
That’s why we’ve started by creating an AI digital bridge between athenahealth and PathSys LIS.
We designed the solution to handle both:
- structured processes – such as athenahealth billing workflows and lab order synchronization,
- unstructured data exchanges – between the PathSys LIS and the billing environment.
We also built our automation in a HIPAA–compliant environment, with encrypted PHI transfer and full audit traceability across both systems.
Here’s what we provided:
Denials Hunter & CPT Code Fixer
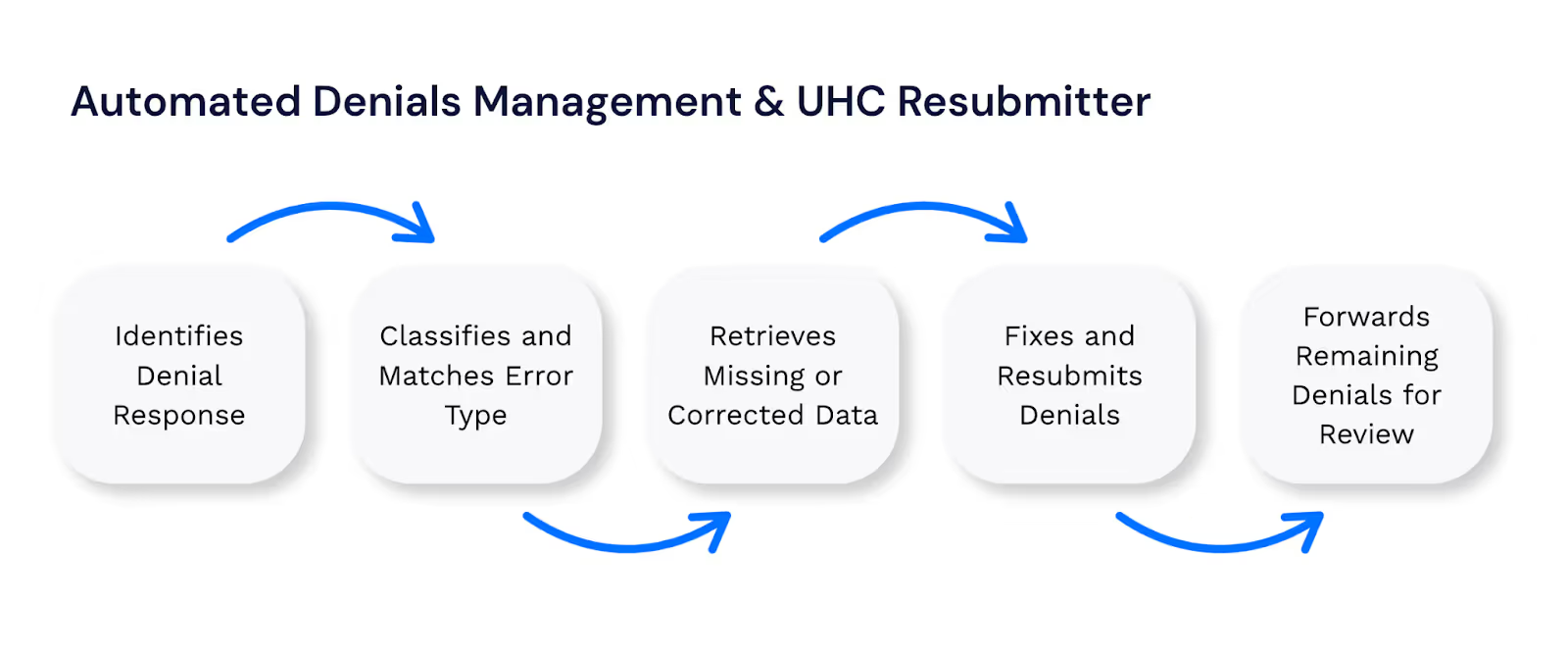
As a second step, we’ve decided to implement a Denial Hunter – an automation that takes over the repetitive and error – prone parts of denials management.
We aimed to find and classify denial types, pull missing or corrected data, fix claims, and resubmit them to payer portals automatically.
In PathGroup's case, 90% of denials are due to minor mistakes, such as eligibility, coverage or incorrect coding issues.
Out of these 90%, a limited number of error types are very repetitive and easy to fix.
We designed the solution to handle both structured billing workflows and unstructured data exchanges between systems. Only sophisticated or unique cases were allowed to end up in human hands.
We ensured the automation could ingest and process new denial records continuously, 24/7.
At the end of the entire process, a summary report is generated showing the ratio of successfully processed cases to all cases handled, which serves as a basic accuracy metric.
How Denial Handling Automation Works?
Impact
The implementation of Denial Hunter unlocked PathGroup’s RCM operations.
Within weeks, the team moved from double-checking spreadsheets to unattended, 24/7 data verification between billing and laboratory systems.
Supported by additional features such as CPT Code Fixer, Laboratory Tests Management Automation, and Patient Registration Automation, our automation reduced the backlog in the targeted denial queues to near-zero levels.
Now, with Denial Hunter and its companion automations running in the background, up to 300 claims per day are automatically verified, corrected, and successfully resubmitted.
But most importantly, PathGroup’s RCM team can finally stay focused on strategic improvements and complex cases that actually require human judgment.
Here are the results:
- Approximately 0.5 FTE saved per month (equivalent to ~6 FTE annually.)
- 200 per day -> 2 per day Initial CPT error rate (roughly),
- Seamless data consistency between PathSys LIS and athenahealth,
- Continuous scalability without additional headcount.
- Claim processing speed: 10 min → 55 sec per case
That’s the power of smart, modular automation – tailored to PathGroup’s architecture, built to grow with their business.
Summary
PathGroup’s journey shows that RCM doesn’t have to be automated all at once.
Smart process automation, even if applied step by step, brings almost instant ROI.
Which brings us to the following point:
We combine proven, ready–to–deploy automations with custom builds – always fitting seamlessly into each client’s existing architecture.
Ready to strengthen your revenue cycle management without growing headcount? Let’s talk!
Let’s talk. In just 15 minutes, we’ll cut through the noise and see if automation works for you.