Hospital margins are under pressure, and revenue cycle inefficiencies are costing providers time and money. In 2023, about 15% of initial claims were denied, up from just 9% in 2016. The cost of handling administrative tasks like prior authorizations can run $6–$11 per claim. For healthcare leaders, this isn’t just a billing issue — it’s a financial imperative. Revenue Cycle Management strategy isn’t about minor tweaks; it’s about rethinking how data, automation, and operations come together to ensure long-term success.
This guide outlines eight core Revenue Cycle Management strategies for building a smarter, faster, and more resilient revenue cycle. From patient intake to collections, we’ll explore how clinics and hospitals can boost revenue performance, especially by leveraging technologies like RPA (Robotic Process Automation) and AI (Artificial Intelligence).
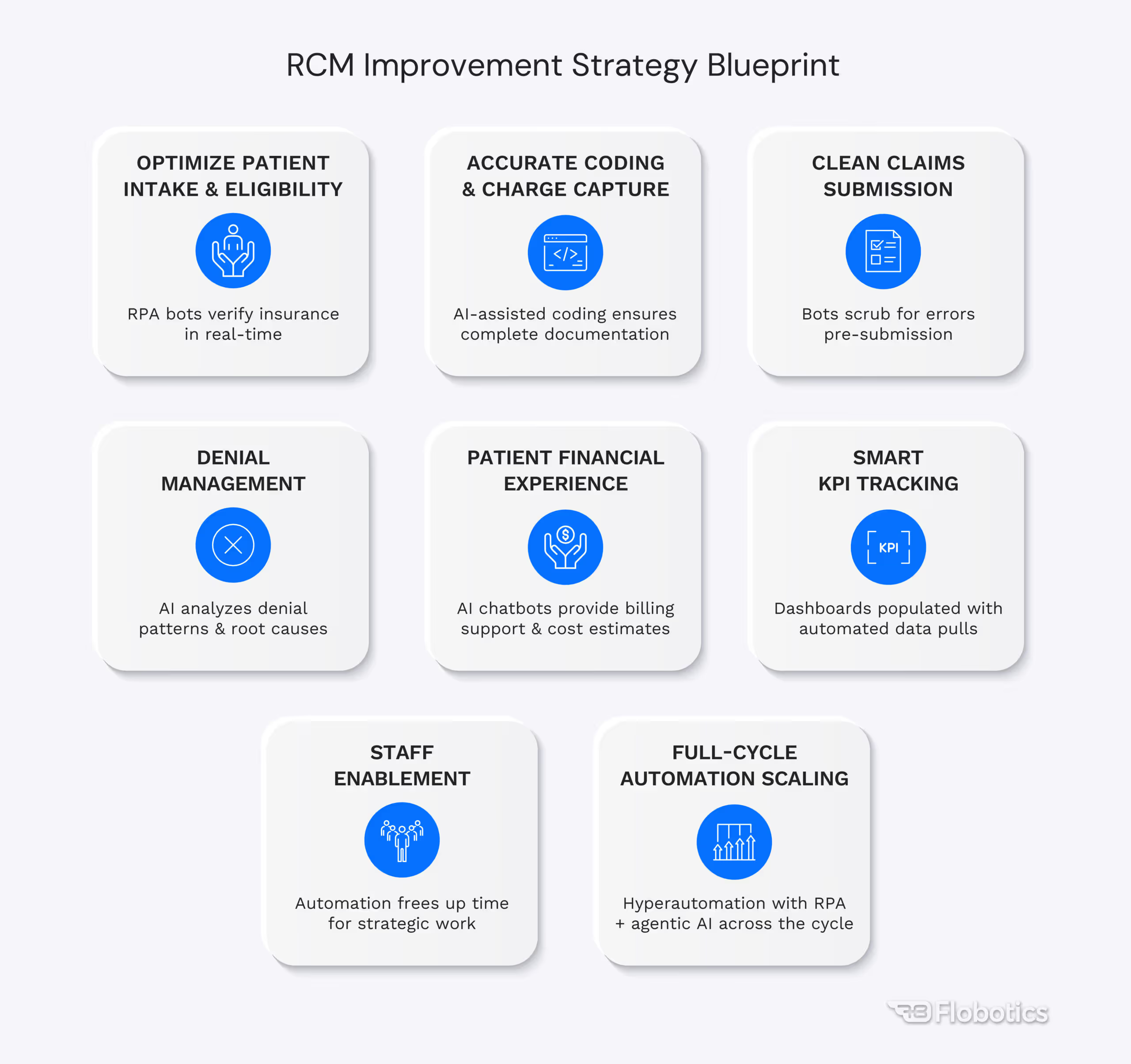
1. Optimize Patient Intake & Eligibility Verification
The revenue cycle starts before a patient ever receives care. Minor errors during patient intake – like a misspelled name, incorrect insurance ID, or missing prior authorization – can snowball into denied claims. Nearly 50% of claim denials stem from front-end issues such as registration/eligibility errors, missing claim data, or lack of pre-certification. These preventable mistakes directly impact cash flow: a claim denied for eligibility is revenue delayed (or lost entirely if not corrected in time).
Why it matters
Getting things right the first time means fewer headaches later. Industry experts advise aiming for a “clean” registration process, where all patient information and coverage details are verified upfront. This foundational step is critical to any effective Revenue Cycle Management strategy, as eliminating front-end errors helps organizations avoid a large portion of denials and the costly rework that follows.
How RPA/AI helps
RPA bots can automatically verify insurance eligibility in real-time as patients are scheduled, checking payer portals to confirm active coverage and benefits. This ensures you catch coverage issues before services are rendered. AI tools can also flag incomplete patient intake forms or prompt staff to collect missing information (like a referral or authorization) during check-in. The result is a smoother intake process with far fewer downstream billing surprises. In short, fixing the front-end with automation sets a solid foundation for your entire Revenue Cycle Management strategy.
2. Ensure Accurate Coding and Documentation
Accurate coding and thorough documentation are the lifeblood of an effective RCM process. Every service must be documented and translated into the correct codes (ICD-10, CPT, etc.) and charges. If something isn’t documented or coded correctly, you won’t get paid for it – it’s that simple. Studies estimate that 1.5–2% of hospital claims fail to capture services that were actually provided. Those are dollars left on the table due to missed charges or coding errors. Additionally, not correcting coding mistakes can lead to denials, underpayments, or even compliance risks.
Why it matters
In an era of tight margins, hospitals and clinics cannot afford to lose revenue due to avoidable documentation mistakes. Strengthening documentation and charge capture processes can have an immediate impact on revenue. For example, rigorous charge capture audits often uncover procedures or tests that were done but not billed. Even a small percentage of missed charges (say 2% of claims) can add up to significant annual revenue loss. Moreover, precise coding ensures you receive the appropriate reimbursement and reduces the chance of claims bouncing back from payers due to coding errors.
How RPA/AI helps
Automation and AI are game-changers for coding and documentation quality. AI-powered computer-assisted coding systems can scan clinical documentation and suggest proper codes, acting as a second set of eyes for human coders. This not only improves accuracy but also speeds up the coding process. RPA bots can assist with charge capture by cross-referencing appointment schedules, procedure logs, and billing systems to make sure every service is accounted for. For instance, if a bot notices a patient had a certain procedure documented in the EMR but no corresponding charge was generated, it can alert staff to investigate, preventing revenue from slipping through the cracks. By coding with precision and leveraging automation, healthcare organizations can significantly reduce denials related to coding and ensure no billable service goes unbilled.
3. Streamline Claims Submission & Tracking
Filing insurance claims promptly and correctly is central to any Revenue Cycle Management strategy. The goal is a high “first-pass” acceptance rate, meaning claims get paid on the first submission without edits or appeals. Every additional touch (resubmitting a claim, calling a payer, etc.) slows cash flow and drives up administrative costs. Industry data shows that roughly 15% of claims are initially denied by insurers, often due to avoidable errors or missing information. Furthermore, once a claim is submitted, the work isn’t over – consistent follow-up is needed to track claim status and handle any issues or delays. This can be incredibly time-consuming if done manually.
Why it matters
Efficient claims submission and follow-up directly impact how quickly your organization gets paid. High-performing RCM teams boast first-pass claim acceptance rates above 90%, which translates to faster reimbursement and fewer write-offs. On the flip side, if your process is sluggish or error-prone, accounts receivable days will balloon. Consider that manually checking the status of claims with payers is estimated to take 17–25 minutes per inquiry, time your staff could spend on more valuable work. Delayed follow-up can also result in missed appeal windows or even timely filing denials, where the insurer refuses payment because the claim wasn’t submitted or corrected in time.
How RPA/AI helps
RPA bots can scrub claims for errors (checking for missing data, invalid codes, or other common denial triggers) before submission, dramatically improving your clean claims rate. Some organizations have seen their first-pass resolution rate climb to 98% with claims automation, meaning almost all claims get approved on first try, leading to faster payments and fewer rework cycles. Additionally, bots can handle the tedious work of claims follow-up: automatically logging into payer websites or clearinghouses to check claim statuses and pulling back detailed info. The bots can even notify your team of pending issues (e.g. a claim that’s stuck or denied) so you can intervene quickly. All of this streamlines the revenue cycle, reduces days in A/R, and improves cash flow. Faster, error-free claims = healthier revenue.
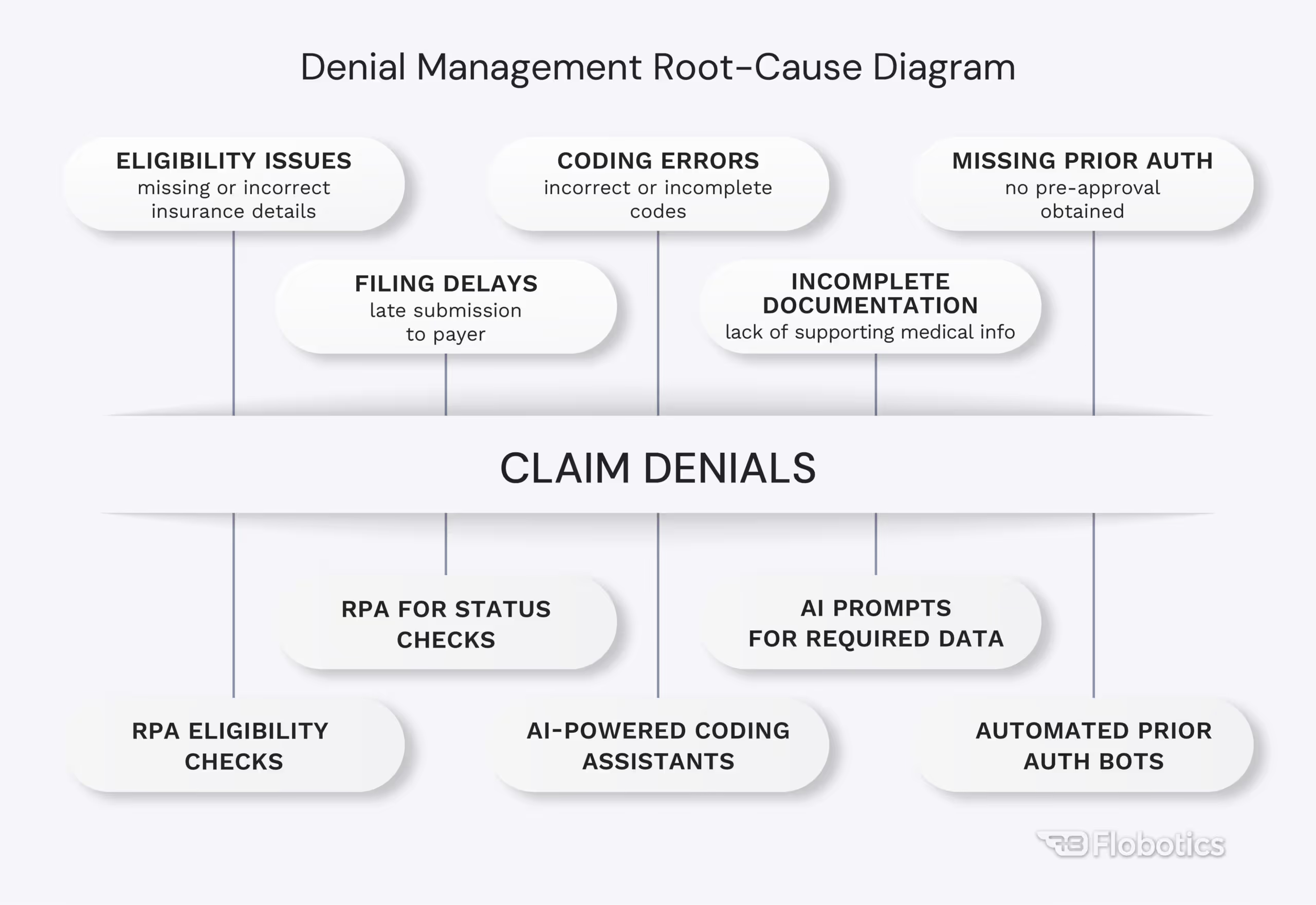
4. Strengthen Denial Management and Collections
Even with the best efforts on the front-end and claims submission, some denials are inevitable. Thus, a strong denial management process is crucial. This means not only working on denials to recover revenue, but also digging into why they occurred so you can prevent similar denials in the future. The scale of the denial problem in healthcare is significant: approximately 10–15% of claims get denied initially on average, and denial rates have been creeping upward yearly (one analysis noted a 15.7% increase in denials from 2020 to 2024). Each denial represents delayed or lost revenue, plus additional cost to appeal or correct the claim.
Why it matters
A high denial rate is essentially a sign of a broken revenue cycle process. Every denial is telling you something – maybe a trend (e.g., many denials from one payer for authorization, or a specific procedure being coded wrong). By analyzing root causes, healthcare leaders can fix systemic issues (like retraining staff on insurance eligibility, correcting a coding problem, or updating documentation protocols). The goal many experts recommend is to keep your denial rate below 5% of claims. Achieving that level requires proactive management and continuous improvement. It’s worth the effort: reducing denials directly boosts revenue and also cuts out waste. Remember, more than half of denials are ultimately preventable through process improvements, especially those stemming from front-end and documentation issues.
How RPA/AI helps
Automation can significantly enhance denial management in two ways: reactive and proactive. On the reactive side, RPA bots can take over much of the manual work of denial processing – for example, retrieving denial codes and details from payer remittances, compiling the documentation needed for an appeal, and even submitting appeal letters through payer portals. This speeds up the response time and ensures no denial “falls through the cracks.”
On the proactive side, AI analytics can sift through your denial data to spot patterns and root causes. Maybe an AI tool finds that a particular insurance company is denying 30% of claims for a certain procedure due to missing prior auth – insight that tells you to tighten your prior authorization checks for that insurer. By acting on root-cause insights, organizations can plug the leaks that cause denials in the first place. In practice, providers that embrace RCM automation report substantial improvements – up to a 30% reduction in denial rates after implementing automated claims and denial management solutions. Fewer denials mean more revenue captured and less money wasted on rework, which is a win-win for your RCM outcomes.
5. Embrace RCM Automation with RPA and AI
Improving Revenue Cycle Management is ultimately a question of strategic resource allocation. Where are your teams spending the most time? Where is revenue slipping through the cracks? And which tasks are ripe for automation without compromising quality or compliance? Revenue Cycle Management strategy like RCM automation — using Robotic Process Automation (RPA) and Artificial Intelligence (AI) — offers a way to reallocate staff effort from manual busywork to high-impact analysis and patient service. While adoption is growing, many organizations still haven’t fully capitalized on automation’s ability to turn inefficient workflows into scalable, tech-enabled systems.
Why It Matters
RPA uses software bots to handle repetitive, rule-based tasks, like checking eligibility, submitting claims, or logging into payer portals, far faster and more accurately than human staff. These bots work 24/7, accelerating workflows and reducing burnout. On the intelligence side, AI adds a new layer of decision-making: Natural Language Processing (NLP) can extract billing codes from clinical notes, machine learning can identify denial patterns, and generative AI can assist in drafting appeal letters or explaining billing.
Real-World Results:
- Auburn Community Hospital used RPA, NLP, and ML to cut 30–35 hours/week of manual appeal writing, improving speed and compliance (AHA).
- Banner Health accelerated insurance discovery with an AI bot that integrated patient coverage into accounts in real time (AHA).
McKinsey estimates that generative AI could reduce total U.S. healthcare spending by 5–10%, or up to $360 billion, mainly by automating administrative functions. Revenue cycle operations — with their high volume of manual tasks — are prime candidates for this transformation. Adopting automation in RCM isn’t as simple as flipping a switch. It takes careful planning, cross-functional alignment, and strong change management. Leaders must establish guardrails to manage AI risks and ensure human oversight. But when implemented strategically, RCM automation improves clean claim rates, lowers denial volumes, shortens reimbursement cycles, and empowers staff to focus on high-value work. It’s more than an operational upgrade — it’s a way to gain a lasting competitive advantage.
6. Enhance the Patient Financial Experience
Today’s healthcare consumers expect a financial experience that is as clear and convenient as any other service they use. From price transparency before care to smooth billing and payment afterward, patient satisfaction now heavily depends on the financial side of their journey. This is not just a nicety – it has real revenue implications. Patients are now responsible for a larger share of healthcare costs, and over 30% of provider revenue often comes directly from patients (through deductibles, co-pays, etc.). If the billing process is confusing or frustrating, those payments may be delayed or lost. Unfortunately, traditional medical billing often falls short: surveys show 74% of patients find medical bills confusing, and 41% of patients are concerned their bills might contain errors, so much so that they may put off paying if they don’t trust the bill’s accuracy. Clearly, there is room to improve the patient financial experience.
Why it matters
A positive patient financial experience can lead to better collection rates and patient loyalty. When patients understand their bills and have easy ways to pay, they’re more likely to pay on time and in full. On the other hand, if bills are late, inaccurate, or opaque, providers may never collect what they’re owed and could even drive patients away. Consider that many patients now shop for healthcare with cost and billing experience in mind. Additionally, patient satisfaction scores are increasingly tied to billing: resolving billing questions and offering convenient payment methods can boost satisfaction ratings by a notable margin (one study cited a 15% increase in satisfaction when billing was clear and easy). In short, treating patients as valued customers in the revenue cycle isn’t just good ethics, it’s good business.
How RPA/AI helps
Automation and AI can significantly enhance the patient’s financial journey. For example, price estimation tools powered by AI can generate an accurate out-of-pocket cost estimate for patients before a procedure, pulling data from insurance contracts and patient benefits. This level of upfront transparency helps patients plan for expenses and reduces surprise bills. On the billing end, RPA can be used to send timely electronic statements and reminders. Chatbots and virtual assistants (often AI-driven) are another powerful tool: they can answer common billing questions 24/7, help patients set up payment plans, or even assist with checking insurance coverage, all without waiting for a phone call. These digital solutions meet patients where they are – on their smartphone or computer – and make the financial process more interactive and less intimidating. Automation can also minimize billing errors (for instance, by cross-verifying charges and payments), which builds patient trust.
7. Leverage Data and KPIs for Continuous Improvement
You can’t improve what you don’t measure. An effective Revenue Cycle Management strategy requires regular tracking of KPIs and data-driven reviews. Rather than managing by gut feeling or anecdote, leading organizations use hard metrics to pinpoint bottlenecks and monitor improvements. There are several foundational RCM metrics every healthcare leader should monitor:
- Days in Accounts Receivable (A/R) (how fast you collect)
- Clean Claim Rate (percentage of claims paid on first submission)
- Denial Rate (percentage of claims denied)
- Net Collection Rate (how much of the owed revenue you actually collect, after adjustments)
- and more.
Tracking these over time and benchmarking against industry standards lets you identify where to focus your improvement efforts. The industry has rallied around data analytics in recent years: FinThrive report found RCM leaders are adopting analytics technology at a very high rate – 80–90% adoption in areas like A/R analytics, claims analytics, and coding analytics. Moreover, in one survey, 76% of healthcare CFOs planned to dedicate at least 10% of their tech budgets to predictive RCM analytics, recognizing the value of data-driven insights. This underscores that data and analytics are no longer optional – they’re a must-have for Reveny Cycle Management strategy.
Why it matters
Regular performance reviews using smart metrics create a continuous feedback loop for your revenue cycle. For instance, by reviewing your denial rate monthly, you might spot an uptick in denials from a particular payer, prompting a root cause analysis before the issue gets worse. Or by monitoring days in A/R, you might notice that one clinic or department lags others, indicating a workflow issue or staffing gap. Data-driven decisions tend to be more effective and targeted. They also help build a business case for investments: if you know your clean claim rate is only 85% and industry best practice is 95 %+, you can quantify how much revenue is stuck in rework and justify spending on training or tools to improve it. The table below highlights a few key RCM metrics and commonly cited performance benchmarks:
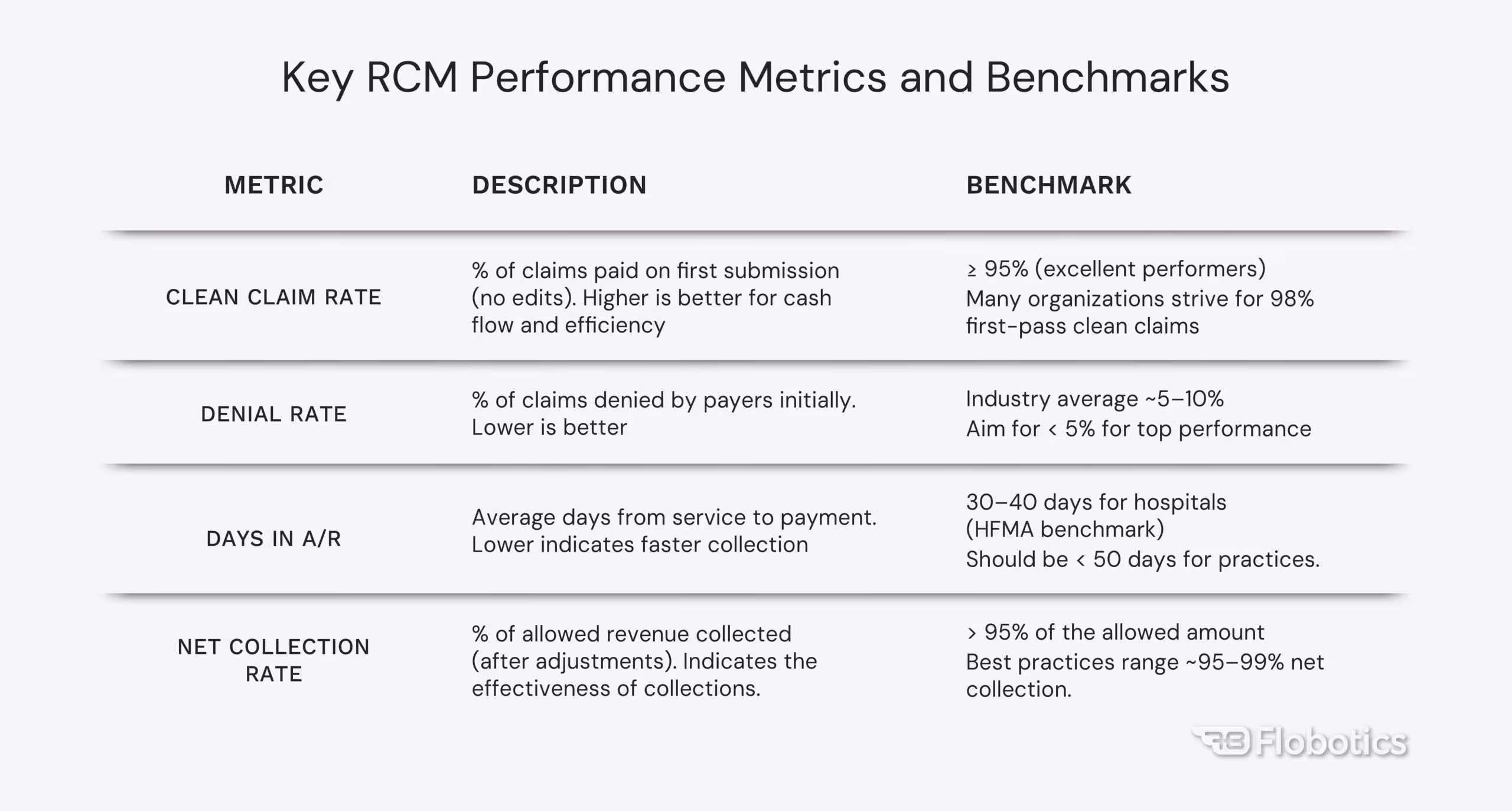
Sources: Clean Claim Rate, Denial Rate, Days in A/R, Net Collection Rate
Healthcare leaders can run data-driven performance reviews monthly or quarterly by keeping a close eye on metrics like these. The data will spotlight where processes are slipping or succeeding. Over time, you can also see the impact of changes (e.g., if a new claims scrubber tool helped raise the clean claim rate, or if a staffing change reduced days in A/R). Celebrating improvements backed by data also boosts team morale – everyone can see the scoreboard.
How RPA/AI helps
RPA can automatically pull data from multiple sources (your EHR, billing system, clearinghouse, etc.) and populate dashboards or reports, saving analysts from tons of spreadsheet work. AI can take it a step further by providing predictive analytics – for example, forecasting next quarter’s cash flow based on current trends, or identifying patterns that human analysts might miss (such as subtle correlations between certain coding practices and denial rates).
Some organizations employ Machine Learning models to predict which claims are most likely to be denied or which patient accounts are at risk of non-payment, allowing staff to prioritize those for intervention. Additionally, business intelligence dashboards can give real-time visibility into metrics across the revenue cycle, so managers aren’t waiting until month-end to spot a problem. The bottom line is that by automating the collection of KPI data and applying AI analytics, providers get actionable insights at their fingertips. This enables proactive management – you can course-correct in weeks or days instead of discovering issues months later.
8. Invest in Team Training and Cross-Functional Collaboration
At the heart of every revenue cycle are the people who make it happen, from front desk registrars and medical coders to billing specialists and denial coordinators. Investing in your RCM staff’s training and fostering cross-functional teamwork can yield significant dividends in efficiency and accuracy. Often, revenue cycle challenges arise not from bad intent but from knowledge gaps or siloed processes. For example, if front-line staff aren’t well-versed in the latest insurance requirements, they might collect incomplete info, leading to denials. Or if billing doesn’t communicate well with clinical departments, there may be disconnects in documentation and coding. When teams are understaffed or under-trained, errors and backlogs increase. Additionally, revenue cycle spans multiple departments, so alignment between them is crucial (hence the term “cross-functional alignment”).
Why it matters
Well-trained, knowledgeable staff can prevent errors before they happen. For instance, training front-end staff on insurance verification can directly reduce eligibility-related denials. Educating clinicians on documentation best practices can lead to more complete charts and fewer coding issues. Cross-functional alignment – such as regular huddles between the billing office, coding team, and clinical managers – ensures that everyone understands how their work impacts the revenue cycle downstream. It breaks down silos. The data supports this holistic approach: front-end knowledge gaps and staff shortages have been cited as major internal factors contributing to higher denials and lower clean claim rates.
Conversely, organizations that emphasize ongoing RCM education and inter-department collaboration often see improvements in metrics like denial rates and days in A/R. In practice, this might involve initiatives like a Revenue Integrity Committee that brings together people from finance, coding, registration, and clinical operations to review performance and tackle issues collectively.
How RPA/AI helps
At first glance, automation might seem unrelated to staff training, but RPA and AI can augment your team and even improve job satisfaction. By automating the most tedious tasks (think copying data from one system to another, or trawling payer sites for claim info), RPA frees your staff to focus on higher-value activities that require human judgment and communication. This shift can make their jobs more fulfilling. It’s notable that 92% of companies reported improved employee satisfaction after implementing AI and RPA solutions, as mundane work was reduced.
In terms of training, AI tools can be used to create smart training programs – for example, using analytics to identify common mistakes and then training staff specifically on those areas. Also, with less time spent on mind-numbing tasks, you can cross-train staff in multiple RCM functions (e.g., a person might get trained in both coding and billing follow-up), building a more flexible team that can cover each other’s duties. Ultimately, people + technology together yield the best results. Invest in your team’s skills and create an environment where automation is viewed as a helpful “digital coworker,” not a threat.
Final Thoughts
Improving RCM is a journey of continuous refinement. These 8 Revenue Cycle Management strategies – from front-end fixes and coding precision to denial analytics and full-cycle automation – provide a roadmap for healthcare leaders to strengthen their RCM processes. The common thread is balancing people, process, and technology. By building a strong process foundation, investing in your team, and amplifying their efforts with RPA and AI, you create a revenue cycle that is efficient, resilient, patient-friendly, and ready for the future. In an industry where financial margins are tight, an optimized revenue cycle management strategy can deliver more than just revenue – it can free your staff to focus on patient care and strategic growth. Here’s to turning these strategies into practice and watching your organization’s financial performance improve, one smart change at a time.
At Flobotics, we specialize in RCM automation. From eligibility checks and claims processing to denial management and prior authorizations, we’ve helped healthcare providers slash costs, reduce errors, and scale operations easily. Let’s discuss how we can improve your Revenue Cycle Management strategy – together.











.jpg)


