You already know this: manual data entry is eating your day alive. Whether you’re running billing, overseeing scheduling, managing claims, or keeping patient records in check, chances are you’re buried in forms, toggling between systems, and fixing avoidable mistakes. The frustrating part? None of it moves the needle for your patients, your bottom line, or your sanity.
That’s where data entry automation comes in. We’re talking about RPA (Robotic Process Automation), AI-powered extraction, OCR, and tight integrations that enable your systems to actually communicate with each other. No more copy-pasting insurance info. No more manually uploading lab results. No more retyping the same patient name into five platforms. With the right tools in place, all of that happens in the background—accurately, securely, and in a fraction of the time.
We’ll break down how automated data entry works in practice and the real-world benefits (from fewer errors to saved hours). Consider this a conversation with a Flobotics automation expert about how to help your team breathe easier, save time, and avoid repeating the same mistakes.
The High Cost of Manual Data Entry in Healthcare
Manual data entry isn’t just an inconvenience – it’s a massive hidden cost. Billing and coding errors alone cost the U.S. healthcare system around $36 billion yearly in lost revenue, denied claims, and penalties. When humans enter codes or billing data, mistakes (such as a mistyped code or an extra zero) can lead to allegations being denied or underpaid, resulting in financial losses for hospitals and clinics.
The impact goes beyond finances. Inaccurate patient records pose a direct risk to patient safety. If a nurse transposes a number in a medication dose or enters a diagnosis code incorrectly, it can result in incorrect treatments or delays. Data integrity failures – such as entering information into the wrong patient’s chart or having out-of-date data in the EHR – can lead to delayed or missed diagnoses, incorrect treatments, and potential patient harm. In healthcare, a simple data entry error can literally be life-threatening.
There’s also a human toll on the workforce. Nurses, doctors, and administrative staff are drowning in digital paperwork. One survey found that staff spend nearly 60% of their time on repetitive tasks, such as data entry and documentation. Think about that – more than half the workweek consumed by updating records, filling forms, and other admin drudgery. This contributes directly to burnout: caregivers feel like data clerks instead of healers. In fact, 37% of healthcare workers say excessive data entry cuts into patient time, and administrative burden is a top driver of workforce burnout. The more hours staff spend typing or fixing errors, the less time they have for patients, leading to frustration, overtime (“pajama time” spent finishing charts), and ultimately, people leaving the profession.
Finally, consider regulatory and compliance risks. Healthcare data is highly sensitive, and manual handling can introduce security gaps. Paper forms and manual re-keying are slow and not secure, leaving organizations vulnerable to HIPAA violations. Every time a staffer manually transcribes patient information, there’s a risk of exposing personal health information or misfiling a record, which can result in compliance fines. In short, the old way of doing things – stacks of forms, copying and pasting between systems, and human error – is enormously costly on all fronts: financially, clinically, and operationally.
What is Data Entry Automation?
So, what do we mean by data entry automation in healthcare? In simple terms, it means utilizing technology, often including RPA bots and AI, to automate the repetitive keystrokes and clicks that humans currently perform. Instead of a medical secretary manually entering referral details from an email into an EHR, for example, a software bot can automatically populate the data into the correct fields. It’s like putting these mundane tasks on autopilot. The goal is for data to move seamlessly from one system to another (such as from a patient intake form to the hospital’s EHR and billing system) without requiring a person to retype it at every step.
It’s important to note that not all automation is created equal. Basic macros or scripts (think of a quick Excel macro) can perform simple, repetitive actions in one application, but they are limited in their capabilities. Modern healthcare data entry automation goes further. RPA bots are essentially the next generation of macros, capable of working across multiple applications and adapting to changes in real-time. Unlike a fixed macro, which only does exactly what it’s programmed to do in one software, an RPA robot can mimic a human’s actions on any software – it can click through a web portal, type into a legacy billing system, or navigate an EHR interface. In practice, RPA software bots “log in” just like a person would and input or transfer information between systems. They mimic human clicks and typing to interact with applications via the user interface, following rules that you set. For example, a bot could be instructed: “Whenever a new patient registration form comes in, pull the name, address, insurance info, etc., and enter them into our EHR.”
Adding Artificial Intelligence takes it up yet another notch. Traditional RPA is rule-based – very effective for structured, repetitive tasks. Combining RPA with AI enables the system to handle unstructured data and make informed decisions. This means tasks that involve reading scanned documents, interpreting text, or making basic decisions (such as flagging an anomaly) can be automated. Simple script automation can handle moving data, but RPA and AI can actually understand it. For instance, AI-powered OCR can read a scanned doctor’s note, and the RPA bot can then extract key details and populate them into the appropriate system. In short, data entry automation ranges from basic to advanced: on one end, there are straightforward scripts for one application; on the other, intelligent bots that navigate entire workflows across EHRs, insurance portals, and billing platforms. The common thread is that your staff aren’t doing the mindless typing – the software for healthcare is.
Top Healthcare Data Entry Processes Ready for Automation
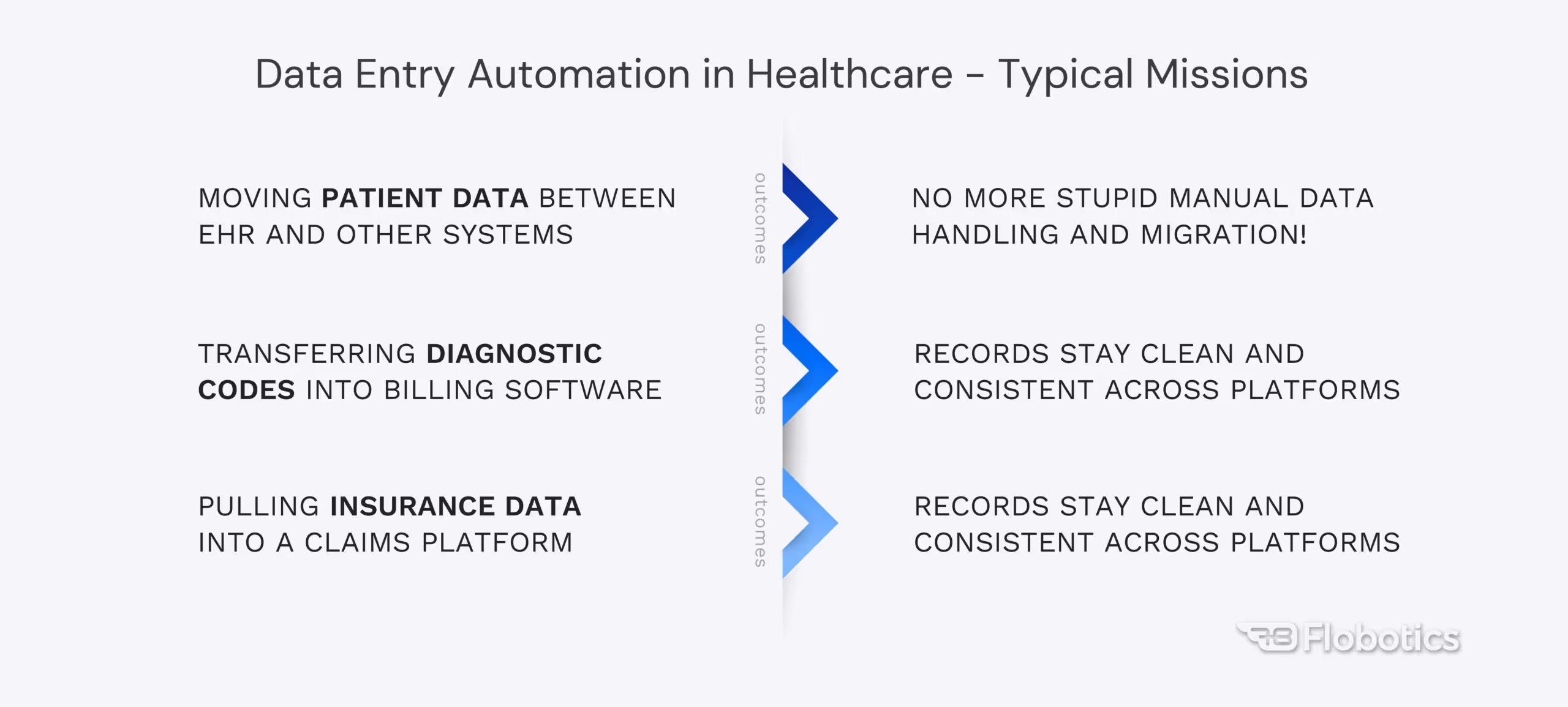
Not every task is ripe for automation, but many are – especially in healthcare, which has no shortage of form-filling and system-hopping. Here are some of the top data entry processes in healthcare that are prime candidates for automation:
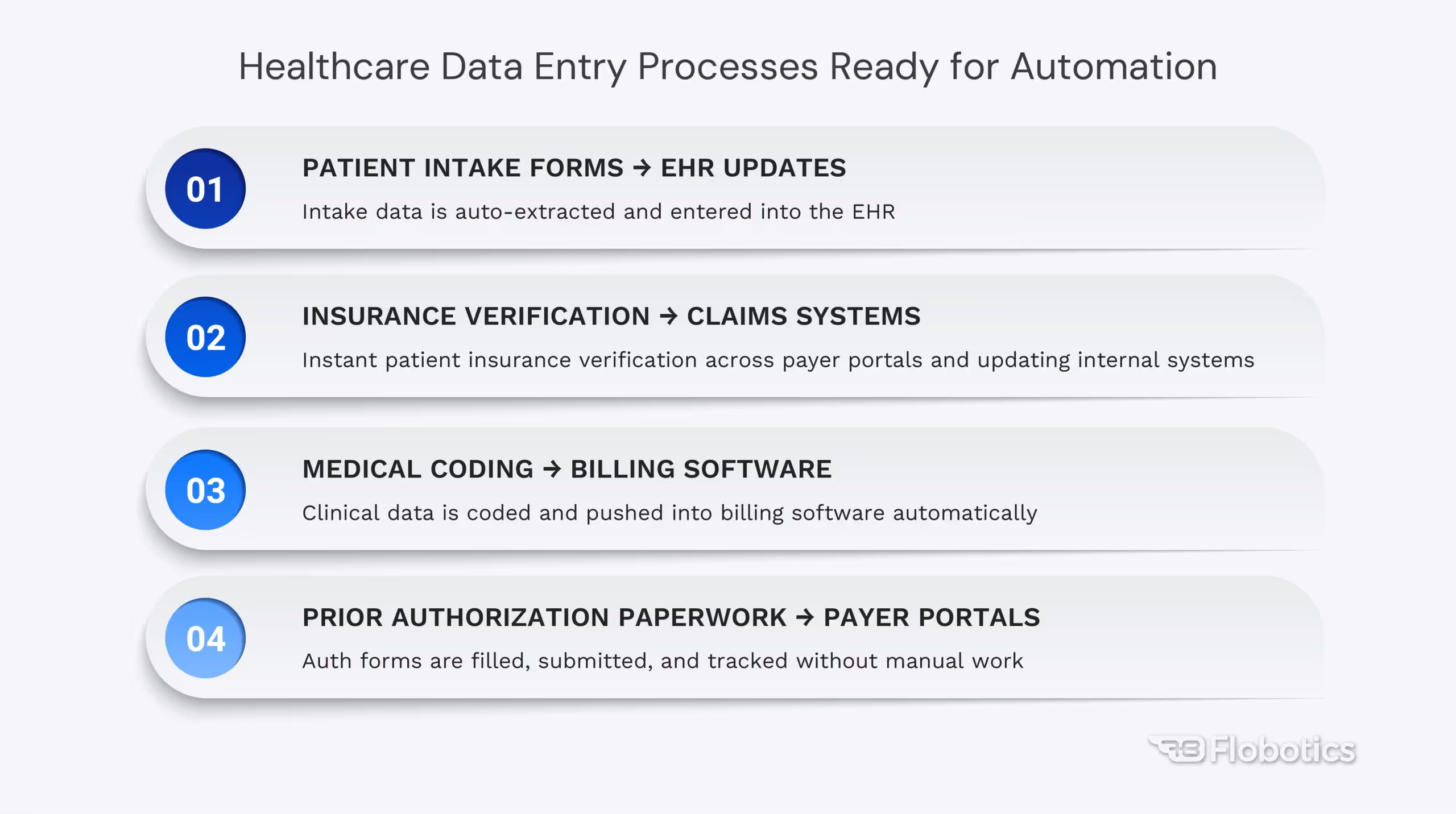
Patient Intake Forms → EHR Updates
From the moment a patient walks in, there’s data to be captured – contact info, medical history, insurance details, you name it. Often, patients fill out digital or paper intake forms, and staff then manually re-enter that information into the Electronic Health Record (EHR). This is tedious and error-prone. Automation can eliminate double entry: for example, scanning/OCR technology can digitize a paper form, and an RPA bot can automatically transfer that data into the EHR fields. The result is faster check-ins and more accurate records. No more deciphering messy handwriting or copying from a clipboard to a computer; the data goes straight from the patient’s form to the system.
Insurance Verification → Claims Systems
Verifying a patient’s insurance eligibility and coverage is a classic repetitive task. Typically, staff log into various payer websites or make phone calls, then input the responses into the practice management or claims system. An automated solution can check insurance eligibility in real time – bots can log into insurance portals (or use integration APIs) to retrieve coverage information and even cross-check the patient’s plan details. The bot then updates the internal system with the verified info (policy active/inactive, co-pay amounts, etc.). This means that insurance verification, which used to take 20+ minutes of hold music and website juggling, can now happen in seconds. By automating insurance checks, healthcare providers see fewer denied claims down the line (since coverage is confirmed upfront) and can process claims much faster.
Medical Coding → Billing Software
Proper coding of diagnoses and procedures is critical for billing and analytics. In many organizations, medical coders or billers spend hours abstracting codes from charts and entering them into billing software. Automation can assist with medical coding by extracting keywords or phrases from clinical documentation (using NLP or OCR) and suggesting appropriate ICD-10 or CPT codes. While full AI coding is still emerging, even partial automation, like a bot that copies physician notes to a coding system or checks codes against a reference database, can save time. Once the codes are determined, an RPA bot can transfer those codes into the billing software or claims form automatically. This reduces coding errors and speeds up the billing cycle because when a doctor finishes a note, a bot could populate the billing system with the requisite codes for charge entry.
Prior Authorization Paperwork → Payer Portals
Prior authorizations (PAs) are a notorious administrative headache – faxing forms, waiting on approvals for medications or procedures. Data entry automation streamlines this by handling the information exchange with insurers. For example, a bot can retrieve the necessary patient information and procedure details from the EHR, complete the payer’s prior authorization request form (often accessed through a web portal or PDF), and submit it electronically. It can then continuously check the payer portal for a determination. The moment approval is granted, the bot grabs the auth number and updates the patient’s record. This end-to-end automation of prior authorizations means providers don’t have to have staff calling insurance companies repeatedly or retyping information into different forms – the bot orchestrates it all. Patients receive their approvals more quickly, and schedulers can proceed with necessary care without administrative delays.
These are just a few examples. Virtually any workflow where staff are “swivel-chairing” between systems – copying data from one screen to another – is a candidate for automated data entry. By targeting processes like the above, healthcare organizations can eliminate some of the most frustrating bottlenecks in their operations.
How Automated Data Entry Works in Healthcare
It sounds almost like magic: information simply “flows” from one system to another. But how does it actually work under the hood? Let’s break down the typical components of an automated data entry workflow in healthcare:
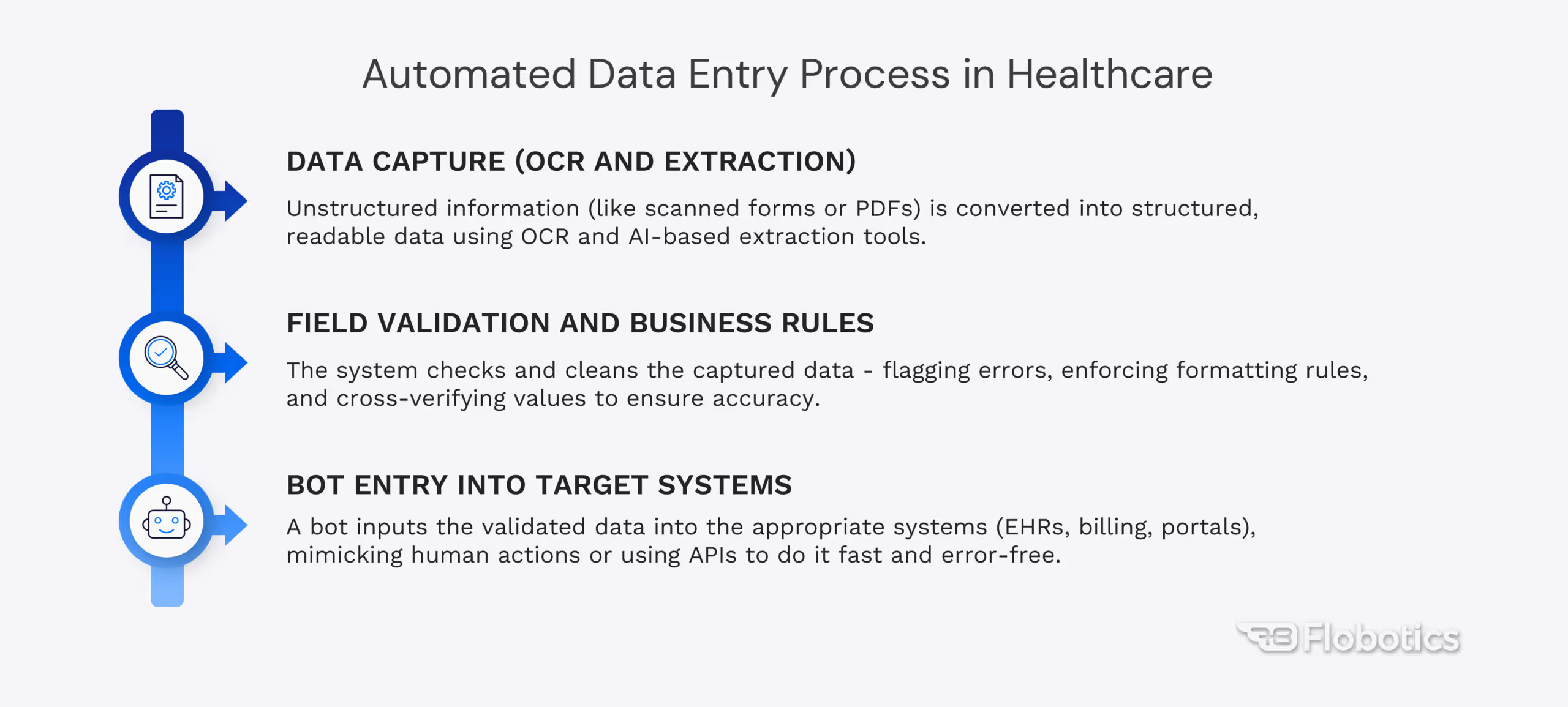
1. Data Capture (OCR and Extraction)
The first step is getting analog or unstructured data into a digital, structured form. For any information that isn’t already electronic – say, a paper form or a fax – automation uses OCR (Optical Character Recognition) to convert it into text. For instance, new patient intake forms or referral letters can be scanned, and OCR software will recognize the text on those pages. Beyond plain OCR, AI-powered data extraction tools can pull specific fields from documents (e.g., patient name, ID number, lab results in a PDF report). The result is that the raw data is now in a usable form (like a data table or JSON) that the bot can work with. This step is like digitizing the input, ensuring the bot “sees” the same data a person would.
2. Field Validation and Business Rules
Once the data is captured, automated workflows apply validation rules just like a diligent human would – only faster. For example, if a date of birth field is captured as 13/25/2025, the system can flag that as invalid. Bots can be programmed to verify that numeric fields contain only numbers, that medical codes have the proper format, or even cross-verify patient identifiers across systems. This ensures that clean, correct data is being entered. Say the OCR misreads an ‘O’ as ‘0’ in an insurance policy number – a validation rule can catch that discrepancy (since the policy format might be known to be letters followed by numbers). By enforcing these checks, automated data entry prevents garbage in and out. Many advanced RPA setups will also cross-reference data, such as whether the patient name on this form matches an existing record. If not, the bot can prompt a review. This validation layer is crucial in healthcare, where compliance and accuracy are paramount.
3. Bot Entry into Target Systems
For the core action, the RPA bot functions as a speedy, error-free data clerk, enabling validated information to be input wherever it is needed. RPA bots can interact with virtually any system or software. They might use APIs when available, but they can also operate through the user interface, mimicking the exact clicks and keystrokes a human would do. For example, a bot could receive a structured dataset (such as a JSON file containing all the fields from a patient intake form) and then launch the hospital’s EHR application. It will navigate to the New Patient screen and systematically fill in name, DOB, address, etc., using the extracted data. It can do this very quickly – no breaks, no typos. Bots can also move data between multiple systems. For example, after updating the EHR, the same bot may log into a billing portal to enter insurance information. Crucially, bots can perform these tasks 24/7 and at high speed, which means overnight, it could update hundreds of records that would take staff days to complete. To illustrate, one RPA system can monitor a folder for incoming patient files and automatically upload that information into the appropriate database or EHR module when a new file appears. In short, the bot “hands off” the data to whatever system needs, with no human in the loop.
Throughout this process, everything the bot does can be logged and audited. That’s a hidden benefit: you get a digital trail of what data was entered, where, and when, which is great for compliance. And if any step fails (say a portal is down), the bot can alert a human or retry automatically. By combining OCR for reading data, AI for interpreting and validating it, and RPA for inputting it, automated data entry creates an end-to-end pipeline: information goes from point A to point B (and C, and D) with minimal human intervention. The result? What used to be an hour of manual copying between systems happens in minutes or less, with near-perfect accuracy.
Key Benefits of Automated Data Entry for Healthcare Ops
Why are healthcare organizations embracing automated data entry? Let’s break down the most significant benefits of introducing some digital horsepower into your workflows. These are the outcomes our Flobotics team sees consistently when we deploy RPA bots in hospitals and clinics:
Fewer Errors, Fewer Headaches
Automation dramatically improves data accuracy. With bots following set rules every time, typos and oversights plunge. Fewer errors mean fewer claim rejections and corrective rework. (Remember that 80% error rate in medical bills? Bots can bring that way down.) The result is lower denial rates and more reliable records, directly boosting your revenue cycle health. Consistent, clean data also keeps you on the right side of compliance.
Time Savings & Higher Productivity
Every minute your staff spend on copy-paste tasks is a minute they’re not helping patients or improving the business. Automated data entry gives you back those minutes (often thousands of hours in aggregate). For instance, one large NHS hospital trust in the UK saved 7,000 staff hours per year by deploying bots to automate their administrative tasks. Closer to home, automation can do routine processes that took days in seconds. Your team can finally tackle the important work on their plate, rather than being overwhelmed by paperwork.
Cost Reduction
When mundane tasks are automated, you simply don’t need as much staff overtime or contractor help to handle peak workloads. That translates to serious cost savings. Across the board, providers save on overhead, spending less money on fixing errors, chasing denials, or hiring temporary workers to clear backlogs. In fact, industry analyses estimate that shifting to automated workflows could save healthcare upwards of $20 billion annually by eliminating inefficiencies.
Improved Staff Morale (No More Soul-Crushing Tasks)
Let’s be honest: data entry drudgery kills morale. When you empower your staff with automation, you’re not replacing them – you’re elevating them to do more meaningful work. Nurses, billing specialists, and admins can focus on patient care, customer service, and problem-solving, rather than punching keys all day. This leads to happier employees and helps combat burnout. Your team can leave on time more often, and they spend their days doing what humans do best, not what bots can do better.
Better Patient Experience
Patients may never see the bots working behind the scenes, but they’ll definitely feel the effects. Automation speeds up turnaround times (e.g., faster insurance checks, quicker billing), so patients get answers and bills sooner and with fewer errors. Fewer mistakes in data entry also mean fewer billing surprises for patients – an accuracy boost that builds trust. Automation creates a more responsive and caring experience for the people you serve by reallocating staff from data-intensive tasks to patient-facing roles.
In summary, automated data entry transforms healthcare operations by attacking the very inefficiencies that have long plagued the industry. It’s about working smarter, not harder – doing more with the resources you have and doing it more accurately. Let’s examine how this transformation unfolds in real life.
Why Flobotics for Healthcare Data Entry Automation?
There’s a growing field of automation providers, but Flobotics stands out regarding healthcare data entry automation. Our approach combines technical expertise with in-depth knowledge of the healthcare domain, which is crucial for success. Here’s why Flobotics is a trusted partner for many healthcare organizations looking to automate their data entry and beyond:
Healthcare-Specific Expertise
We’re not generalists dabbling in healthcare; Flobotics has dedicated healthcare RPA specialists who understand the nuances of medical workflows, billing cycles, and compliance requirements. Healthcare Revenue Cycle Management, claims processing, HL7 integration, HIPAA privacy rules – our team speaks your language. This means we design automation solutions that fit your reality.
Rapid Deployment
We have a proven framework for identifying quick-win processes and deploying ready-to-use bots in under 30 days in many cases. Whether it’s automating patient onboarding or claim form entry, we strive to get a pilot up and running in a month or less – and then scale from there.
Scalability and Flexibility
Flobotics solutions are built to grow with you. We often start with one or two high-impact processes (for example, automating data entry for prior auths or referrals), and once you see the value, scaling up is straightforward. Do you need to add more bots during peak season? Do you need to extend automation to a new department? No problem. Our approach utilizes modular, reusable bot components and a robust orchestration platform, enabling quick and cost-efficient addition of capacity or new workflows.
End-to-End Support and Partnership
We don’t just drop off a piece of software and leave. Flobotics prides itself on being a true partner in your automation journey. We’ve got you covered, from initial process discovery (identifying which data entry tasks will yield the best return on investment) to development, testing, and ongoing maintenance. In healthcare, where rules and systems are constantly evolving, we stay by your side to update and optimize your automations. Flobotics combines the latest technology (AI, OCR, RPA) with a human-centric approach to ensure the automation works in your context.
From Data Chaos to Streamlined Care
Picture your operations a few months after implementing automated data entry: forms flow effortlessly between systems, patient records update instantly, claims go out error-free on the first try, and your team finally has breathing room. The compliance department isn’t chasing missing information, and finance isn’t writing off as many denied claims. In short, your whole organization can breathe easier.
With the right automation partner and a clear roadmap, you can start small, perhaps automating one painfully slow data entry task, and then scale up. It’s about working alongside your existing software, supercharging your staff with a digital workforce that handles the boring stuff.
Ready to put data entry on autopilot? Flobotics specializes in helping healthcare teams implement automation smoothly and effectively. We’ve walked in your shoes and understand the unique challenges of healthcare ops. Schedule a free consulting session with our healthcare automation experts to see how automated data entry could work in your environment – we’ll even show you a live demo of a bot in action. Let’s talk about plugging your leaks in time and accuracy, and map out a step-by-step plan to get you from chaos to calm.











.jpg)


